Fibrinolysis is the natural process that breaks down blood clots to maintain healthy blood flow and prevent blockages in your vessels. Understanding how this mechanism works is crucial for managing conditions like thrombosis and promoting overall cardiovascular health. Explore the article to learn more about fibrinolysis and its role in your body's defense system.
Table of Comparison
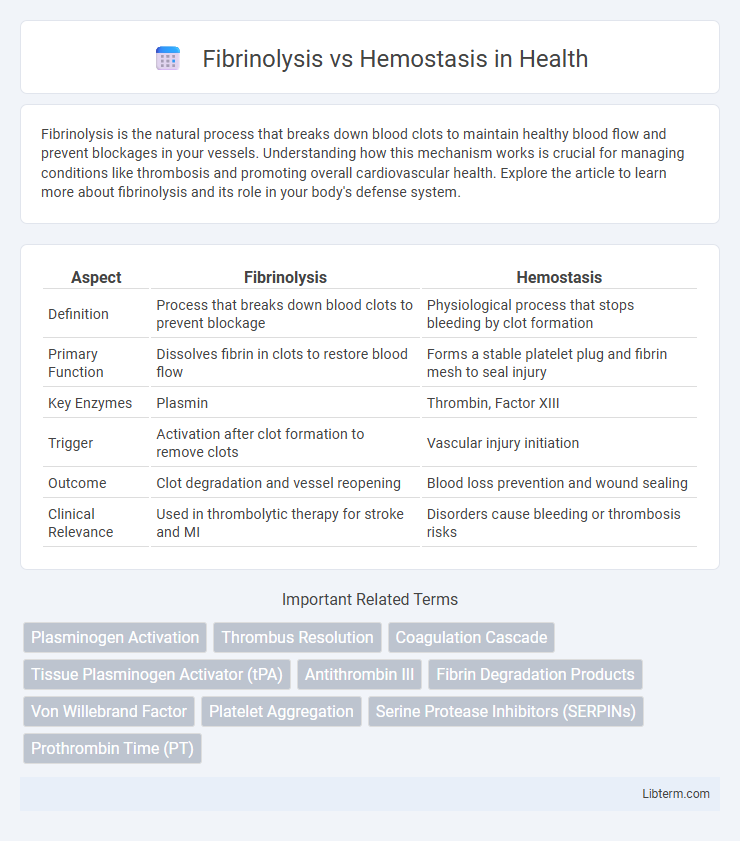
| Aspect | Fibrinolysis | Hemostasis |
|---|---|---|
| Definition | Process that breaks down blood clots to prevent blockage | Physiological process that stops bleeding by clot formation |
| Primary Function | Dissolves fibrin in clots to restore blood flow | Forms a stable platelet plug and fibrin mesh to seal injury |
| Key Enzymes | Plasmin | Thrombin, Factor XIII |
| Trigger | Activation after clot formation to remove clots | Vascular injury initiation |
| Outcome | Clot degradation and vessel reopening | Blood loss prevention and wound sealing |
| Clinical Relevance | Used in thrombolytic therapy for stroke and MI | Disorders cause bleeding or thrombosis risks |
Introduction to Fibrinolysis and Hemostasis
Fibrinolysis is the physiological process that breaks down fibrin clots, maintaining vascular patency and preventing thrombosis, whereas hemostasis encompasses the complex cascade of vascular, platelet, and coagulation factors that stop bleeding by forming a stable clot. Hemostasis initiates immediately after vascular injury through vasoconstriction, platelet activation, and the coagulation cascade, culminating in fibrin mesh formation. Fibrinolysis involves plasmin activation, which degrades fibrin clots, balancing clot formation to avoid excessive thrombosis and ensuring normal blood flow.
Overview of Hemostasis: The Body’s First Line of Defense
Hemostasis is the body's immediate response to vascular injury, initiating a tightly regulated process to prevent excessive bleeding by forming a stable blood clot. It involves vascular constriction, platelet aggregation, and activation of the coagulation cascade, culminating in fibrin mesh formation to seal the wound. This primary defense mechanism maintains blood vessel integrity while balancing clot formation and dissolution to prevent thrombosis, distinguishing it from fibrinolysis, which functions to break down clots after healing.
The Process and Phases of Hemostasis
Hemostasis is a vital physiological process that prevents excessive bleeding following vascular injury through three main phases: vascular spasm, platelet plug formation, and coagulation. During vascular spasm, blood vessels constrict to reduce blood flow, while platelet plug formation involves platelet adhesion, activation, and aggregation to form a temporary seal at the injury site. The coagulation phase stabilizes the platelet plug by converting fibrinogen into fibrin, creating a durable clot that secures tissue repair until fibrinolysis subsequently breaks down the clot to restore normal blood flow.
Understanding Fibrinolysis: Breaking Down Clots
Fibrinolysis is a critical physiological process that breaks down blood clots, preventing excessive clot formation and maintaining vascular health. It involves the activation of plasminogen to plasmin, an enzyme that degrades fibrin, the primary structural component of clots. Understanding fibrinolysis enhances insights into hemostasis, the overall clotting mechanism that balances clot formation and dissolution to prevent bleeding and thrombosis.
Key Enzymes and Factors in Hemostasis
Hemostasis involves key enzymes and factors such as thrombin, fibrinogen, and factor XIII that facilitate clot formation and stabilization. Platelet activation releases ADP and thromboxane A2, promoting aggregation, while tissue factor initiates the coagulation cascade leading to fibrin mesh formation. In contrast, fibrinolysis primarily depends on plasminogen activation to plasmin, which degrades fibrin and dissolves blood clots, balancing hemostatic processes.
Major Players in Fibrinolysis
The major players in fibrinolysis include plasminogen, tissue plasminogen activator (tPA), and plasmin, which work together to break down fibrin clots and maintain vascular patency. Plasminogen is converted into plasmin by tPA, initiating fibrin degradation and preventing excessive clot formation. In contrast, hemostasis primarily involves platelets, clotting factors, and thrombin to form stable blood clots and stop bleeding.
Differences between Fibrinolysis and Hemostasis
Fibrinolysis is the biological process that breaks down blood clots by degrading fibrin, while hemostasis is the physiological mechanism that stops bleeding by forming clots through platelet aggregation and fibrin mesh formation. Hemostasis involves vasoconstriction, platelet plug formation, and coagulation cascade activation to stabilize blood vessel injury, whereas fibrinolysis activates plasmin to dissolve clots after tissue repair is complete. The key difference lies in their functions: hemostasis initiates clot formation to prevent hemorrhage, and fibrinolysis ensures clot removal to restore normal blood flow.
Physiological Importance of Balance between Hemostasis and Fibrinolysis
The physiological balance between hemostasis and fibrinolysis is crucial for maintaining vascular integrity and preventing pathological conditions such as thrombosis or excessive bleeding. Hemostasis involves platelet aggregation and fibrin clot formation to stop bleeding, while fibrinolysis ensures timely clot dissolution by plasmin-mediated degradation of fibrin. Disruptions in this balance can lead to disorders like deep vein thrombosis or hemorrhagic diseases, highlighting the importance of regulatory mechanisms controlling coagulation and fibrinolytic pathways.
Clinical Disorders Related to Hemostasis and Fibrinolysis
Hemostasis disorders such as hemophilia and von Willebrand disease disrupt clot formation, leading to excessive bleeding, while fibrinolysis abnormalities, including hyperfibrinolysis and plasminogen activator inhibitor-1 (PAI-1) deficiency, cause excessive clot breakdown and bleeding tendencies. Thrombosis, related to impaired fibrinolysis, results from insufficient clot degradation, contributing to conditions like deep vein thrombosis and pulmonary embolism. Effective management of these clinical disorders requires precise diagnostic evaluation of coagulation and fibrinolytic pathways to tailor anticoagulant or procoagulant therapies.
Therapeutic Interventions Targeting Hemostasis and Fibrinolysis
Therapeutic interventions targeting hemostasis primarily involve anticoagulants like heparin and warfarin, which inhibit clot formation to prevent thrombosis. Fibrinolysis is modulated using agents such as tissue plasminogen activator (tPA) and streptokinase that promote clot breakdown, critical in treating acute ischemic strokes and myocardial infarctions. Novel therapies also include direct thrombin inhibitors and antifibrinolytic drugs like tranexamic acid, balancing the dynamic regulation between clot formation and dissolution.
Fibrinolysis Infographic
 libterm.com
libterm.com