Dystonic conditions cause involuntary muscle contractions that lead to repetitive movements or abnormal postures, often affecting the neck, face, or limbs. Understanding the symptoms and treatment options can improve quality of life significantly. Explore the rest of the article to learn how you can manage or support someone with dystonia effectively.
Table of Comparison
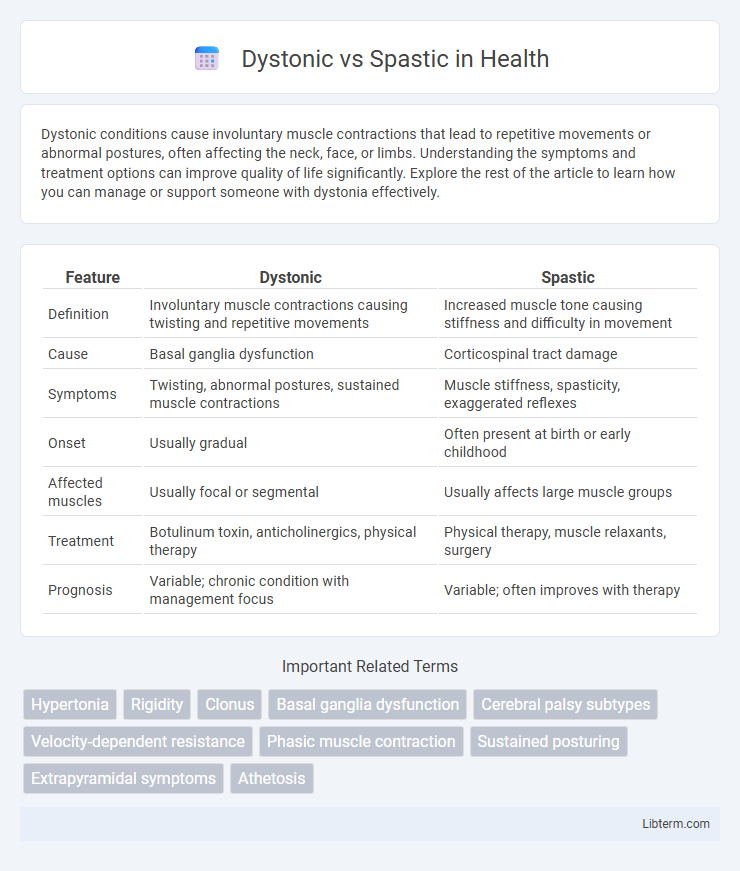
| Feature | Dystonic | Spastic |
|---|---|---|
| Definition | Involuntary muscle contractions causing twisting and repetitive movements | Increased muscle tone causing stiffness and difficulty in movement |
| Cause | Basal ganglia dysfunction | Corticospinal tract damage |
| Symptoms | Twisting, abnormal postures, sustained muscle contractions | Muscle stiffness, spasticity, exaggerated reflexes |
| Onset | Usually gradual | Often present at birth or early childhood |
| Affected muscles | Usually focal or segmental | Usually affects large muscle groups |
| Treatment | Botulinum toxin, anticholinergics, physical therapy | Physical therapy, muscle relaxants, surgery |
| Prognosis | Variable; chronic condition with management focus | Variable; often improves with therapy |
Understanding Dystonia and Spasticity: Key Differences
Dystonia involves involuntary muscle contractions causing twisting and repetitive movements or abnormal postures, often triggered by neurological dysfunction in the basal ganglia. Spasticity, characterized by increased muscle tone and hyperactive stretch reflexes, results from upper motor neuron lesions affecting the corticospinal tract. Understanding these key neurological and clinical differences is crucial for accurate diagnosis and targeted treatment strategies.
Causes and Risk Factors of Dystonic and Spastic Disorders
Dystonic disorders are primarily caused by dysfunctions in the basal ganglia, often linked to genetic mutations, brain injuries, or exposure to certain medications like antipsychotics. Spastic disorders typically result from damage to the upper motor neurons, frequently seen in conditions such as cerebral palsy, multiple sclerosis, or stroke. Both dystonic and spastic disorders share risk factors including neurological trauma, infections, and inherited genetic abnormalities that disrupt normal muscle control pathways.
Clinical Features: How Dystonic and Spastic Movements Differ
Dystonic movements are characterized by sustained muscle contractions causing twisting and repetitive motions, often leading to abnormal postures, while spastic movements involve increased muscle tone and stiffness resulting in jerky or clumsy motions. Clinically, dystonia manifests as involuntary, patterned, and often task-specific muscle contractions, whereas spasticity presents with velocity-dependent resistance to passive stretch and hyperactive deep tendon reflexes. Differentiating these features aids in diagnosing neurological conditions such as dystonia and spastic cerebral palsy.
Neurological Mechanisms: Underlying Pathways
Dystonic movements result from abnormal signaling within the basal ganglia, particularly disruptions in the cortico-striato-pallido-thalamo-cortical loop, leading to involuntary muscle contractions and sustained postures. Spasticity originates from upper motor neuron lesions affecting the corticospinal tract, causing hyperexcitability of the stretch reflex and increased muscle tone. These distinct neurological mechanisms explain the differing clinical presentations, with dystonia reflecting central motor circuit dysfunction and spasticity involving impaired inhibition of spinal reflexes.
Diagnostic Approaches: Identifying Dystonia vs Spasticity
Differentiating dystonia from spasticity involves clinical assessment of movement patterns and muscle tone, where dystonia presents with involuntary, sustained muscle contractions causing twisting and repetitive movements, while spasticity is characterized by velocity-dependent increased muscle tone and hyperreflexia. Electromyography (EMG) aids in distinguishing these by revealing co-contraction of agonist and antagonist muscles in dystonia versus increased reflex activity in spasticity. Neuroimaging techniques, such as MRI, support diagnosis by identifying underlying lesions typical of spasticity, often linked to upper motor neuron damage, contrasting with the basal ganglia dysfunction associated with dystonia.
Impact on Motor Function and Daily Life
Dystonic movements cause involuntary muscle contractions leading to twisting and repetitive motions, severely impairing precise motor function and coordination required for daily tasks. Spasticity results in muscle stiffness and exaggerated reflexes, restricting range of motion and making activities like walking or grasping objects challenging. Both conditions disrupt fine and gross motor skills, significantly reducing independence and quality of life.
Therapeutic Strategies: Managing Dystonic vs Spastic Symptoms
Therapeutic strategies for managing dystonic symptoms often include anticholinergic medications, botulinum toxin injections, and physical therapy aimed at reducing muscle contractions and improving motor control. In contrast, spastic symptom management emphasizes muscle relaxants like baclofen or tizanidine, intrathecal baclofen therapy, and targeted physical and occupational therapy to enhance range of motion and reduce hypertonia. Both conditions benefit from multidisciplinary approaches that tailor interventions to individual symptom severity and functional goals.
Rehabilitation Techniques for Dystonic and Spastic Patients
Rehabilitation techniques for dystonic patients often include sensory retraining, task-specific exercises, and botulinum toxin injections combined with physical therapy to reduce involuntary muscle contractions and improve motor control. Spastic patients benefit from stretching, strength training, electrical stimulation, and constraint-induced movement therapy to enhance muscle function and reduce hypertonia. Both conditions require individualized rehabilitation plans incorporating neuroplasticity principles and functional mobility training to maximize patient outcomes.
Prognosis and Long-Term Outcomes
Dystonic disorders often exhibit variable prognoses depending on the underlying cause, with some patients experiencing progressive worsening while others maintain stable symptoms over time. Spastic conditions, commonly linked to spastic cerebral palsy or spinal cord injuries, tend to have more predictable outcomes related to muscle stiffness and mobility impairments but may improve with consistent physical therapy and medical interventions. Long-term management of both dystonic and spastic disorders requires multidisciplinary approaches to optimize function, reduce complications, and enhance quality of life.
Recent Advances and Future Directions in Treatment
Recent advances in the treatment of dystonic and spastic disorders emphasize gene therapy, deep brain stimulation (DBS), and personalized rehabilitation protocols targeting specific neural circuits. Emerging pharmacological agents, such as selective ion channel modulators and neuroinflammatory pathway inhibitors, demonstrate promising efficacy in reducing aberrant muscle contractions and improving motor function. Future directions include the integration of biomarker-driven precision medicine and adaptive neuromodulation technologies to enhance therapeutic outcomes and minimize side effects.
Dystonic Infographic
 libterm.com
libterm.com