Sjogren's syndrome is a chronic autoimmune disorder characterized by the immune system attacking moisture-producing glands, leading to dry eyes and mouth. This condition can also cause joint pain, swelling, and fatigue, significantly impacting your daily life and overall health. Discover more about symptoms, diagnosis, and treatment options in the rest of this article.
Table of Comparison
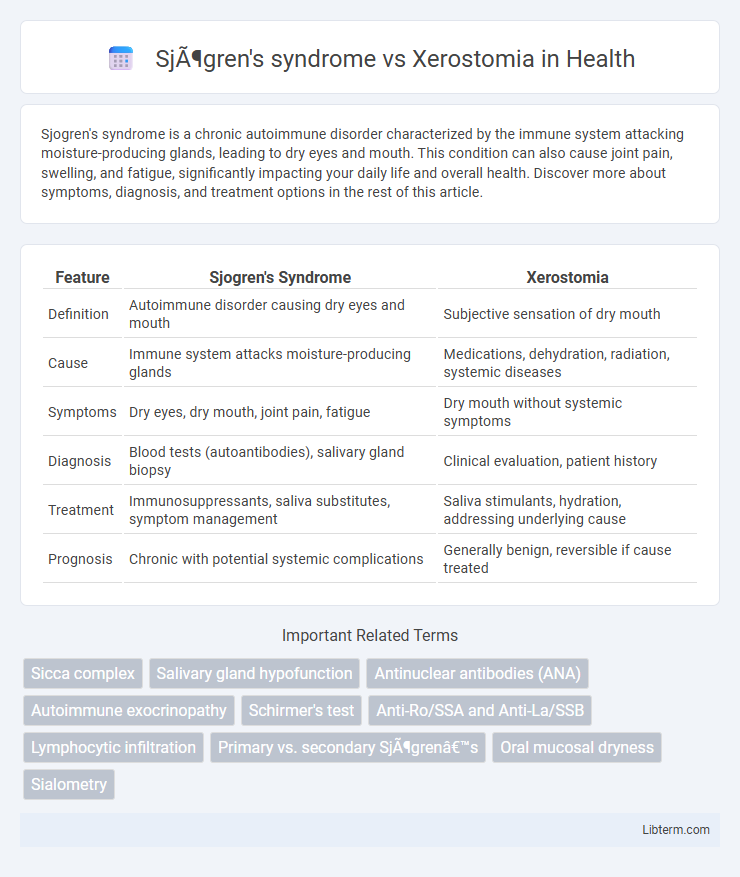
| Feature | Sjogren's Syndrome | Xerostomia |
|---|---|---|
| Definition | Autoimmune disorder causing dry eyes and mouth | Subjective sensation of dry mouth |
| Cause | Immune system attacks moisture-producing glands | Medications, dehydration, radiation, systemic diseases |
| Symptoms | Dry eyes, dry mouth, joint pain, fatigue | Dry mouth without systemic symptoms |
| Diagnosis | Blood tests (autoantibodies), salivary gland biopsy | Clinical evaluation, patient history |
| Treatment | Immunosuppressants, saliva substitutes, symptom management | Saliva stimulants, hydration, addressing underlying cause |
| Prognosis | Chronic with potential systemic complications | Generally benign, reversible if cause treated |
Introduction to Sjögren's Syndrome and Xerostomia
Sjogren's syndrome is a chronic autoimmune disorder primarily characterized by lymphocytic infiltration of the exocrine glands, leading to dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca). Xerostomia, a subjective sensation of oral dryness, can result from various causes including medication side effects, radiation therapy, and systemic diseases like Sjogren's syndrome. Distinguishing Sjogren's syndrome from other causes of xerostomia requires clinical evaluation, serologic testing for autoantibodies (anti-Ro/SSA and anti-La/SSB), and salivary gland biopsy for accurate diagnosis.
Understanding the Definition of Sjögren's Syndrome
Sjogren's syndrome is a chronic autoimmune disorder characterized by the immune system attacking the body's moisture-producing glands, primarily the salivary and lacrimal glands, leading to dry mouth and dry eyes. Unlike xerostomia, which is a symptom referring specifically to dry mouth caused by various factors such as medication or dehydration, Sjogren's syndrome is an underlying systemic condition with widespread autoimmune involvement. Diagnosis involves serological tests detecting autoantibodies like anti-Ro/SSA and anti-La/SSB, distinguishing it from simple xerostomia.
What is Xerostomia?
Xerostomia, commonly known as dry mouth, is a condition characterized by decreased saliva production, leading to dryness in the oral cavity. It often results from medication side effects, radiation therapy, or systemic diseases, distinct from Sjogren's syndrome, which is an autoimmune disorder causing chronic dryness due to salivary gland inflammation. Understanding xerostomia's etiology is crucial for targeted treatment, as it impacts oral health, increasing the risk of dental caries and mucosal infections.
Key Differences Between Sjögren's Syndrome and Xerostomia
Sjogren's syndrome is an autoimmune disorder characterized by chronic inflammation of salivary and lacrimal glands, leading to dry mouth (xerostomia) and dry eyes, whereas xerostomia refers specifically to the subjective sensation of dry mouth, which can result from multiple causes including medication, radiation therapy, or systemic diseases. Unlike xerostomia alone, Sjogren's syndrome involves systemic manifestations such as arthritis, fatigue, and increased risk of lymphoma, confirmed by serologic markers like anti-Ro/SSA and anti-La/SSB antibodies. Diagnosis of Sjogren's requires clinical, serological, and histopathological criteria, while xerostomia diagnosis typically involves symptom evaluation and salivary flow measurement without systemic involvement.
Causes of Sjögren's Syndrome vs. Xerostomia
Sjogren's syndrome is an autoimmune disorder where the immune system attacks moisture-producing glands, primarily targeting salivary and lacrimal glands, leading to dry mouth and eyes. Xerostomia, or dry mouth, is commonly caused by medication side effects, radiation therapy, dehydration, or systemic diseases but is not always linked to autoimmune activity. Unlike xerostomia, Sjogren's syndrome involves chronic inflammation and glandular dysfunction driven by autoimmune mechanisms.
Common Symptoms: Overlapping and Distinct
Sjogren's syndrome and xerostomia both present with dry mouth as a primary symptom, but Sjogren's syndrome also involves systemic manifestations such as dry eyes, joint pain, and fatigue. Xerostomia, often caused by medication or radiation therapy, primarily affects salivary gland function without the autoimmune inflammatory component seen in Sjogren's syndrome. The overlap includes oral dryness and difficulty swallowing, while distinct signs of Sjogren's include positive anti-SSA/Ro antibodies and lymphocytic infiltration in salivary glands confirmed by biopsy.
Diagnostic Criteria for Both Conditions
Sjogren's syndrome diagnosis relies on the American-European Consensus Group criteria, including positive anti-SSA/Ro or anti-SSB/La antibodies, salivary gland biopsy showing focal lymphocytic sialadenitis, and objective evidence of reduced salivary flow or ocular dryness. Xerostomia diagnosis primarily involves patient-reported symptoms of dry mouth and clinical evaluation of salivary gland function without the systemic autoimmune markers found in Sjogren's syndrome. Salivary flow rate tests, sialography, and serologic tests differentiate Sjogren's syndrome from xerostomia, with Sjogren's exhibiting systemic autoimmune activity versus xerostomia's diverse etiologies like medication side effects or dehydration.
Treatment Approaches: Sjögren's Syndrome vs. Xerostomia
Treatment approaches for Sjogren's syndrome primarily include immunosuppressive medications such as hydroxychloroquine and corticosteroids to address systemic autoimmune inflammation, alongside saliva substitutes and secretagogues like pilocarpine to relieve dry mouth symptoms. Xerostomia management focuses mainly on symptomatic relief using artificial saliva, good oral hygiene, and hydration, with pilocarpine or cevimeline prescribed cautiously when gland function remains viable. Both conditions benefit from multidisciplinary care involving rheumatologists, dentists, and oral medicine specialists for optimized treatment outcomes.
Prognosis and Long-Term Management
Sjogren's syndrome prognosis varies based on systemic involvement, with increased risk for lymphoma and chronic organ complications requiring regular monitoring and tailored immunosuppressive therapy. Xerostomia, often a symptom of underlying conditions or medication side effects, typically involves management focused on symptom relief using saliva substitutes and stimulants to prevent dental caries and oral infections. Long-term management of both conditions emphasizes maintaining oral health through rigorous hygiene, regular dental visits, and addressing systemic factors contributing to salivary gland dysfunction.
When to Seek Medical Evaluation
Seek medical evaluation for Sjogren's syndrome when persistent dry mouth is accompanied by dry eyes, joint pain, or prolonged fatigue, as these systemic symptoms suggest an autoimmune disorder. Xerostomia alone warrants medical attention if dryness disrupts speech, swallowing, or contributes to frequent dental cavities, indicating potential underlying causes like medication side effects or salivary gland dysfunction. Early assessment by a healthcare provider enables appropriate diagnosis through antibody tests and salivary gland imaging, facilitating timely management to prevent complications.
Sjögren's syndrome Infographic
 libterm.com
libterm.com