Ataxia manifests as a lack of muscle coordination, often leading to difficulties with balance and speech, which differs from paralysis characterized by the loss of muscle function. Understanding the distinctions between ataxia and paralysis is crucial for accurate diagnosis and effective treatment strategies. Explore the full article to learn how these neurological conditions impact your health and the available options for management.
Table of Comparison
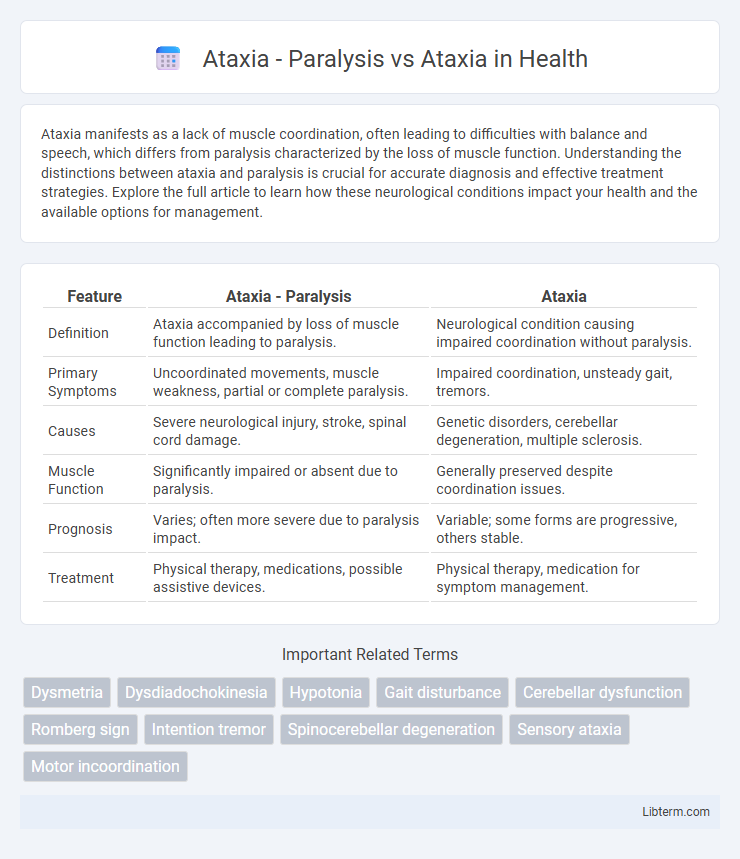
| Feature | Ataxia - Paralysis | Ataxia |
|---|---|---|
| Definition | Ataxia accompanied by loss of muscle function leading to paralysis. | Neurological condition causing impaired coordination without paralysis. |
| Primary Symptoms | Uncoordinated movements, muscle weakness, partial or complete paralysis. | Impaired coordination, unsteady gait, tremors. |
| Causes | Severe neurological injury, stroke, spinal cord damage. | Genetic disorders, cerebellar degeneration, multiple sclerosis. |
| Muscle Function | Significantly impaired or absent due to paralysis. | Generally preserved despite coordination issues. |
| Prognosis | Varies; often more severe due to paralysis impact. | Variable; some forms are progressive, others stable. |
| Treatment | Physical therapy, medications, possible assistive devices. | Physical therapy, medication for symptom management. |
Introduction to Ataxia and Paralysis
Ataxia is a neurological condition characterized by impaired coordination, balance, and speech due to dysfunction in the cerebellum or sensory pathways. Paralysis involves the loss of muscle function in part of the body, often caused by nerve damage, spinal cord injury, or stroke. While ataxia affects movement precision and control, paralysis results in the complete or partial inability to move muscles, distinguishing their symptoms and underlying mechanisms.
Defining Ataxia: Causes and Symptoms
Ataxia is a neurological disorder characterized by impaired coordination, balance, and speech, resulting from damage to the cerebellum or its pathways. Causes of ataxia include genetic mutations, stroke, multiple sclerosis, alcohol abuse, and vitamin deficiencies. Symptoms typically involve unsteady gait, difficulty with fine motor tasks, slurred speech, and involuntary eye movements, differentiating it from paralysis, which is marked by loss of muscle function rather than coordination issues.
Paralysis: Types and Clinical Features
Paralysis associated with ataxia manifests in various forms including flaccid, spastic, and monoplegia, each displaying distinct clinical features such as muscle weakness, loss of voluntary movement, and altered reflexes. Flaccid paralysis is characterized by reduced muscle tone and absent reflexes, often resulting from peripheral nerve or lower motor neuron damage. Spastic paralysis involves increased muscle tone and hyperactive reflexes, originating from upper motor neuron lesions, while monoplegia is paralysis confined to one limb, highlighting localized neurological impairment.
Key Differences Between Ataxia and Paralysis
Ataxia primarily involves the loss of coordination and balance due to cerebellar dysfunction, characterized by unsteady gait and clumsiness, while paralysis refers to the complete loss of muscle function in one or more parts of the body due to nerve damage. Ataxia affects motor control without causing muscle weakness, whereas paralysis results in an inability to voluntarily move the affected muscles. Diagnosis of ataxia typically involves neurological examination and imaging to assess cerebellar damage, while paralysis often requires nerve conduction studies and muscle strength tests to identify the extent and location of nerve or spinal cord injury.
Neurological Mechanisms of Ataxia vs Paralysis
Ataxia results from dysfunction in the cerebellum or its pathways, leading to impaired coordination, balance, and motor control without muscle weakness. Paralysis involves damage to motor neurons or corticospinal tracts, causing loss of voluntary muscle movement and strength. Neurologically, ataxia affects proprioceptive inputs and cerebellar processing, while paralysis disrupts motor signal transmission from the brain to muscles.
Diagnostic Approaches for Ataxia and Paralysis
Diagnostic approaches for ataxia primarily involve neurological examinations, MRI scans to detect cerebellar degeneration or lesions, and genetic testing to identify hereditary ataxias such as Friedreich's ataxia or spinocerebellar ataxia. In contrast, paralysis diagnosis often requires electromyography (EMG) and nerve conduction studies to assess muscle and nerve function, alongside imaging techniques like CT or MRI to identify causes such as stroke, spinal cord injury, or nerve compression. Cerebrospinal fluid analysis and blood tests support differential diagnosis by excluding infections or autoimmune conditions contributing to ataxia or paralysis.
Common Conditions Associated with Ataxia
Ataxia is commonly associated with neurological disorders such as multiple sclerosis, cerebellar degeneration, and stroke, which impair coordination and balance. Paralysis, often resulting from spinal cord injury or stroke, primarily affects muscle strength and voluntary movement but can coexist with ataxia when lesions involve cerebellar pathways. Both conditions highlight the impact of central nervous system damage on motor function, emphasizing the importance of accurate diagnosis for effective management.
Treatment Strategies: Ataxia vs Paralysis
Treatment strategies for ataxia primarily focus on physical therapy to improve coordination, occupational therapy to enhance daily functioning, and addressing underlying causes such as vitamin deficiencies or autoimmune disorders. In contrast, paralysis treatment emphasizes restoring muscle function through nerve stimulation, physical rehabilitation, and in some cases, surgical interventions or assistive devices. Both conditions benefit from multidisciplinary approaches, but ataxia management targets motor control and balance, while paralysis treatment centers on muscle strength restoration and mobility support.
Prognosis and Patient Outcomes
Ataxia characterized by paralysis often indicates severe neural impairment, resulting in poorer prognosis and increased risk of long-term disability compared to non-paralytic ataxia. Patients with non-paralytic ataxia typically experience more favorable functional outcomes, benefiting from targeted rehabilitation and neuroplasticity. Early diagnosis and multidisciplinary management are critical in improving prognosis and minimizing complications in both ataxic conditions.
Quality of Life: Living with Ataxia or Paralysis
Living with ataxia involves managing coordination difficulties and balance problems, which impact daily activities but often allow for some independence. Paralysis causes complete or partial loss of muscle function, significantly restricting mobility and increasing dependence on caregiving and assistive devices. Both conditions affect quality of life profoundly, with tailored rehabilitation and support systems playing critical roles in enhancing functional abilities and emotional well-being.
Ataxia - Paralysis Infographic
 libterm.com
libterm.com