Hyponatremia is a condition characterized by low sodium levels in the blood, which can cause symptoms ranging from mild confusion to severe neurological issues. Proper diagnosis and management are crucial to prevent complications such as seizures or coma. Explore the rest of the article to learn how you can recognize symptoms and understand effective treatment options for hyponatremia.
Table of Comparison
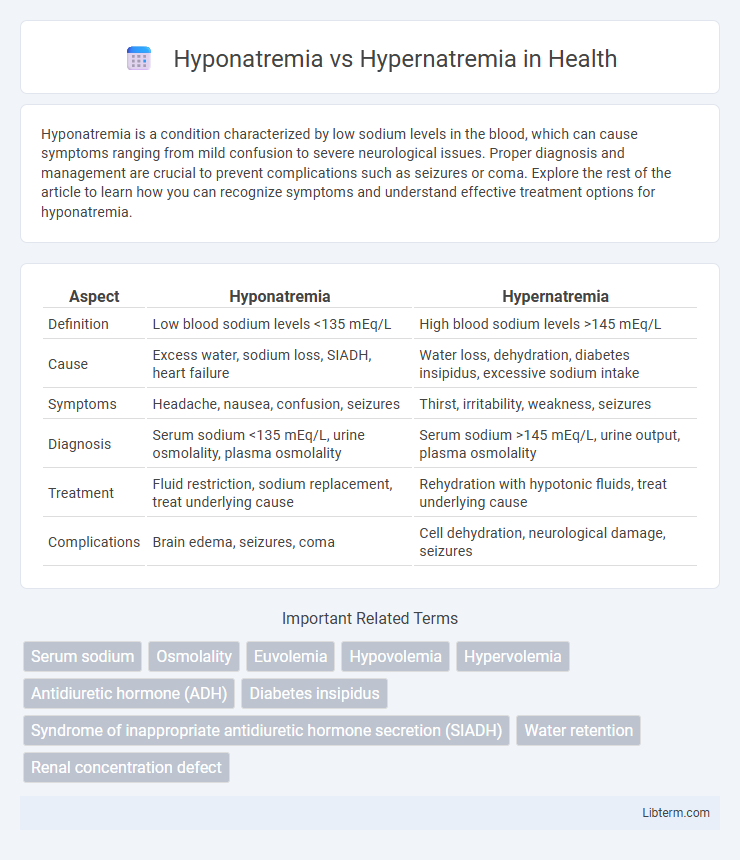
| Aspect | Hyponatremia | Hypernatremia |
|---|---|---|
| Definition | Low blood sodium levels <135 mEq/L | High blood sodium levels >145 mEq/L |
| Cause | Excess water, sodium loss, SIADH, heart failure | Water loss, dehydration, diabetes insipidus, excessive sodium intake |
| Symptoms | Headache, nausea, confusion, seizures | Thirst, irritability, weakness, seizures |
| Diagnosis | Serum sodium <135 mEq/L, urine osmolality, plasma osmolality | Serum sodium >145 mEq/L, urine output, plasma osmolality |
| Treatment | Fluid restriction, sodium replacement, treat underlying cause | Rehydration with hypotonic fluids, treat underlying cause |
| Complications | Brain edema, seizures, coma | Cell dehydration, neurological damage, seizures |
Introduction to Sodium Imbalance
Sodium imbalance is a critical condition characterized by abnormal levels of sodium in the blood, primarily manifesting as hyponatremia or hypernatremia. Hyponatremia occurs when serum sodium concentration falls below 135 mEq/L, leading to cellular swelling and neurological disturbances, while hypernatremia is defined by serum sodium levels exceeding 145 mEq/L, causing cellular dehydration and potential neurological impairment. Both conditions reflect disruptions in water and electrolyte homeostasis, necessitating precise diagnosis and management to prevent severe complications.
Hyponatremia: Definition and Causes
Hyponatremia is a medical condition characterized by abnormally low sodium levels in the blood, typically below 135 mmol/L, leading to cellular swelling and neurological symptoms. Common causes include excessive fluid intake, heart failure, kidney disease, and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Understanding the etiology of hyponatremia is crucial for prompt diagnosis and tailored treatment to prevent complications like cerebral edema.
Hypernatremia: Definition and Causes
Hypernatremia is characterized by an elevated sodium concentration in the blood exceeding 145 mmol/L, typically caused by water loss or excessive sodium intake. Common causes include dehydration from diarrhea, diabetes insipidus, and hyperaldosteronism, leading to an imbalance in fluid regulation. This condition disrupts cellular homeostasis, resulting in neurological symptoms like confusion, seizures, or coma if untreated.
Risk Factors for Sodium Disorders
Hyponatremia risk factors include excessive fluid intake, heart failure, liver cirrhosis, and use of diuretics or antidepressants that alter sodium balance. Hypernatremia often results from dehydration, impaired thirst mechanism in the elderly, diabetes insipidus, or excessive sodium intake. Both conditions are prevalent in hospitalized patients with underlying kidney disease, sepsis, or neurological disorders affecting water and sodium homeostasis.
Signs and Symptoms: Hyponatremia vs Hypernatremia
Hyponatremia typically presents with symptoms such as headache, nausea, confusion, seizures, and muscle cramps due to low serum sodium levels disrupting cellular function. Hypernatremia is characterized by thirst, lethargy, irritability, muscle twitching, and in severe cases, seizures or coma, resulting from elevated sodium concentrations causing cellular dehydration. Recognizing these distinct clinical manifestations is crucial for timely diagnosis and management of sodium imbalances.
Diagnostic Approaches for Sodium Imbalance
Diagnostic approaches for sodium imbalance begin with precise measurement of serum sodium levels, where hyponatremia is defined by sodium concentrations below 135 mmol/L and hypernatremia by levels exceeding 145 mmol/L. Comprehensive evaluation includes assessment of urine osmolality and urine sodium to distinguish between hypovolemic, euvolemic, and hypervolemic states, with urine sodium typically low (<20 mmol/L) in hypovolemia and high (>40 mmol/L) in renal salt wasting or euvolemic hyponatremia. Additional laboratory tests such as serum osmolality and assessments of adrenal and thyroid function support differential diagnosis and guide targeted management strategies.
Complications Associated with Sodium Disorders
Hyponatremia often leads to cerebral edema, seizures, and in severe cases, respiratory arrest due to water shifting into brain cells. Hypernatremia can cause cellular dehydration, resulting in neurological deficits, muscle weakness, and increased risk of intracranial hemorrhage. Both sodium imbalances pose significant risks to neurological function and require prompt medical intervention to prevent long-term complications.
Treatment Strategies for Hyponatremia
Treatment strategies for hyponatremia primarily involve correcting low serum sodium levels through careful fluid management and addressing underlying causes such as SIADH, heart failure, or renal impairment. Administration of hypertonic saline, typically 3% sodium chloride, is reserved for severe symptomatic cases to rapidly increase sodium concentration while avoiding osmotic demyelination syndrome by limiting correction rates to no more than 8-10 mmol/L in 24 hours. Fluid restriction, salt tablets, or vasopressin receptor antagonists like tolvaptan are commonly employed to manage chronic or less severe hyponatremia by promoting water excretion and restoring sodium balance.
Treatment Strategies for Hypernatremia
Treatment strategies for hypernatremia primarily involve gradual correction of serum sodium levels through controlled administration of hypotonic fluids such as 5% dextrose in water or half-normal saline to prevent cerebral edema. Frequent monitoring of serum electrolytes and fluid balance is critical to avoid rapid shifts in sodium concentration. Addressing the underlying cause, whether it is excessive water loss or sodium overload, is essential for effective management.
Prevention and Long-Term Management
Preventing hyponatremia involves maintaining adequate sodium intake and monitoring fluid balance, especially in vulnerable populations such as the elderly and athletes. Long-term management emphasizes regular electrolyte monitoring, individualized fluid restrictions, and addressing underlying causes like heart, kidney, or liver disorders to avoid recurrence. Hypernatremia prevention centers on ensuring sufficient water intake, particularly in patients with impaired thirst mechanisms, while chronic management includes gradual sodium correction and management of conditions affecting water retention and loss.
Hyponatremia Infographic
 libterm.com
libterm.com