Neutropenia and lymphocytopenia are conditions characterized by abnormally low levels of neutrophils and lymphocytes, respectively, which play crucial roles in your immune system's defense against infections. These blood disorders can lead to increased vulnerability to infections and may signal underlying health issues that require medical evaluation. Discover more about the causes, symptoms, and treatments of neutropenia and lymphocytopenia in the rest of this article.
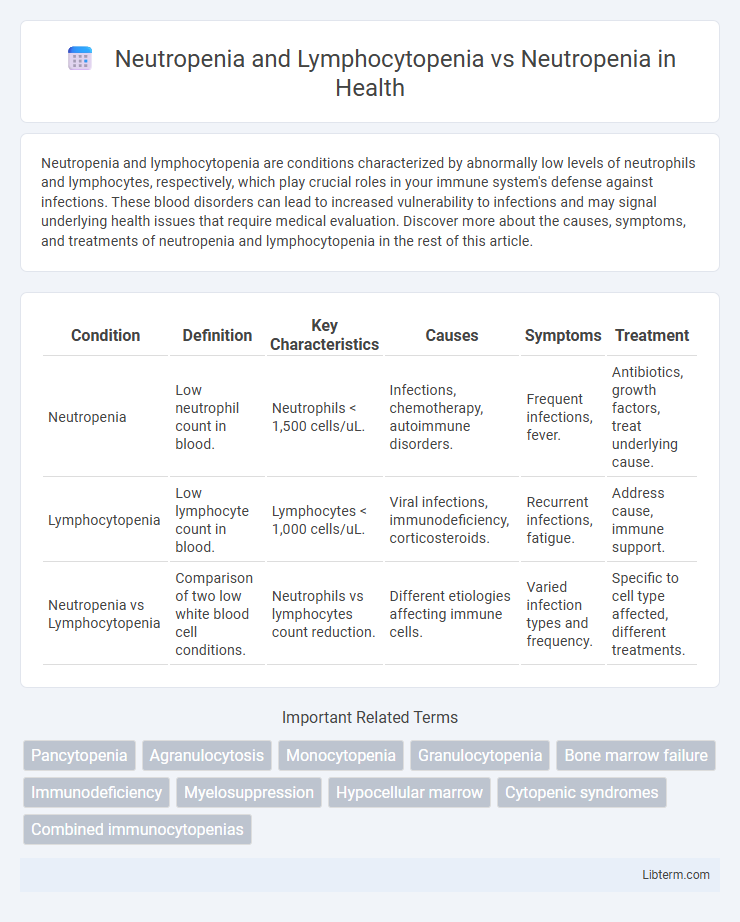
Table of Comparison
| Condition | Definition | Key Characteristics | Causes | Symptoms | Treatment |
|---|---|---|---|---|---|
| Neutropenia | Low neutrophil count in blood. | Neutrophils < 1,500 cells/uL. | Infections, chemotherapy, autoimmune disorders. | Frequent infections, fever. | Antibiotics, growth factors, treat underlying cause. |
| Lymphocytopenia | Low lymphocyte count in blood. | Lymphocytes < 1,000 cells/uL. | Viral infections, immunodeficiency, corticosteroids. | Recurrent infections, fatigue. | Address cause, immune support. |
| Neutropenia vs Lymphocytopenia | Comparison of two low white blood cell conditions. | Neutrophils vs lymphocytes count reduction. | Different etiologies affecting immune cells. | Varied infection types and frequency. | Specific to cell type affected, different treatments. |
Introduction to Neutropenia and Lymphocytopenia
Neutropenia and lymphocytopenia are hematological conditions characterized by abnormally low levels of neutrophils and lymphocytes, respectively, key components of the immune system. Neutropenia primarily increases susceptibility to bacterial infections, while lymphocytopenia compromises adaptive immunity, affecting viral and certain bacterial defense mechanisms. Understanding the distinct pathophysiology and clinical implications of neutropenia and lymphocytopenia is essential for accurate diagnosis and tailored treatment strategies in immunocompromised patients.
Defining Neutropenia: Causes and Clinical Significance
Neutropenia is defined by an abnormally low count of neutrophils, crucial white blood cells that defend against bacterial and fungal infections. Causes include bone marrow disorders, chemotherapy, autoimmune diseases, and severe infections, which suppress neutrophil production or increase destruction. Clinically, neutropenia significantly raises infection risk, necessitating prompt diagnosis and management to prevent severe complications.
Exploring Lymphocytopenia: Overview and Etiology
Lymphocytopenia, characterized by an abnormally low lymphocyte count, often coexists with neutropenia but represents a distinct immunodeficiency impacting adaptive immunity, particularly T and B cells. Etiologies of lymphocytopenia include viral infections such as HIV, autoimmune diseases, chemotherapy, and certain genetic disorders, differentiating it from neutropenia primarily caused by bacterial infections or bone marrow suppression. Understanding lymphocytopenia's specific causes and immunological impact is critical for accurate diagnosis and tailored treatment strategies in patients presenting with combined or isolated cytopenias.
Neutropenia vs Neutropenia and Lymphocytopenia: Core Differences
Neutropenia involves a decreased neutrophil count, primarily impacting bacterial infection defense, while neutropenia combined with lymphocytopenia signifies reductions in both neutrophils and lymphocytes, affecting broader immune functions including viral and malignancy-related responses. Neutropenia alone often indicates bone marrow suppression or acute infection, whereas the dual cytopenia suggests more severe immunodeficiency or systemic disease processes such as HIV or hematologic malignancies. Clinical management and prognostic outcomes differ significantly, with neutropenia plus lymphocytopenia requiring more comprehensive diagnostic evaluation and aggressive immunomodulatory therapies.
Risk Factors Associated with Each Condition
Neutropenia is primarily linked to risk factors such as chemotherapy, bone marrow disorders, and infections that suppress neutrophil production, increasing susceptibility to bacterial infections. Lymphocytopenia is often associated with viral infections, autoimmune diseases, and immunodeficiency syndromes, leading to impaired adaptive immunity and heightened risk of viral and opportunistic infections. While neutropenia mainly compromises innate immune response against bacteria, lymphocytopenia impacts adaptive immunity, influencing susceptibility to a broader range of pathogens.
Diagnostic Approaches: CBC and Beyond
Diagnostic approaches for neutropenia and lymphocytopenia primarily involve a complete blood count (CBC) with differential, which quantifies neutrophil and lymphocyte levels to identify deficiencies. Beyond CBC, flow cytometry enhances lymphocyte subset analysis, while bone marrow biopsy provides insight into hematopoietic function critical for diagnosing underlying causes. Molecular testing and serological assays further aid in detecting infections or genetic disorders associated with these cytopenias, ensuring a precise diagnostic framework.
Clinical Manifestations: Similarities and Contrasts
Neutropenia and lymphocytopenia both present with increased susceptibility to infections, reflecting compromised immune defenses, yet neutropenia predominantly leads to bacterial and fungal infections due to reduced neutrophil counts, while lymphocytopenia increases vulnerability to viral, fungal, and opportunistic infections caused by diminished lymphocyte populations. Clinical manifestations of neutropenia often include fever, mouth ulcers, and skin infections, whereas lymphocytopenia may exhibit signs related to viral reactivation such as cytomegalovirus or Epstein-Barr virus infections, along with increased risk for certain malignancies. Overlapping features include general fatigue and malaise, but contrasting immune cell deficits dictate the specific pathogen susceptibility and infection patterns observed in patients.
Management Strategies for Neutropenia Alone
Management strategies for neutropenia primarily involve prompt identification of infection risks and implementation of prophylactic antibiotics or antifungals to prevent severe complications. Use of granulocyte colony-stimulating factor (G-CSF) accelerates neutrophil recovery, especially in chemotherapy-induced neutropenia. Regular monitoring of absolute neutrophil count (ANC) guides treatment adjustments and helps reduce hospitalization and mortality rates.
Therapeutic Considerations for Combined Neutropenia and Lymphocytopenia
Therapeutic considerations for combined neutropenia and lymphocytopenia require tailored immunomodulatory strategies to address increased susceptibility to opportunistic infections due to dual immune cell deficits. Prophylactic antimicrobials, granulocyte colony-stimulating factor (G-CSF), and lymphocyte-supportive agents such as interleukin-7 or immunoglobulin replacement therapy are integral to management. Close monitoring of infection markers and immune function guides treatment adjustments to reduce morbidity and optimize immune reconstitution in patients with overlapping neutropenia and lymphocytopenia.
Prognosis and Long-Term Outcomes
Neutropenia combined with lymphocytopenia often indicates a more severe underlying immunodeficiency, leading to a poorer prognosis and increased risk of opportunistic infections compared to isolated neutropenia. Long-term outcomes for patients with both conditions typically involve higher morbidity due to impaired innate and adaptive immune responses, necessitating closer monitoring and aggressive management. In contrast, isolated neutropenia usually presents a better prognosis with fewer complications, although risks depend on severity and etiology.
Neutropenia and Lymphocytopenia Infographic
 libterm.com
libterm.com