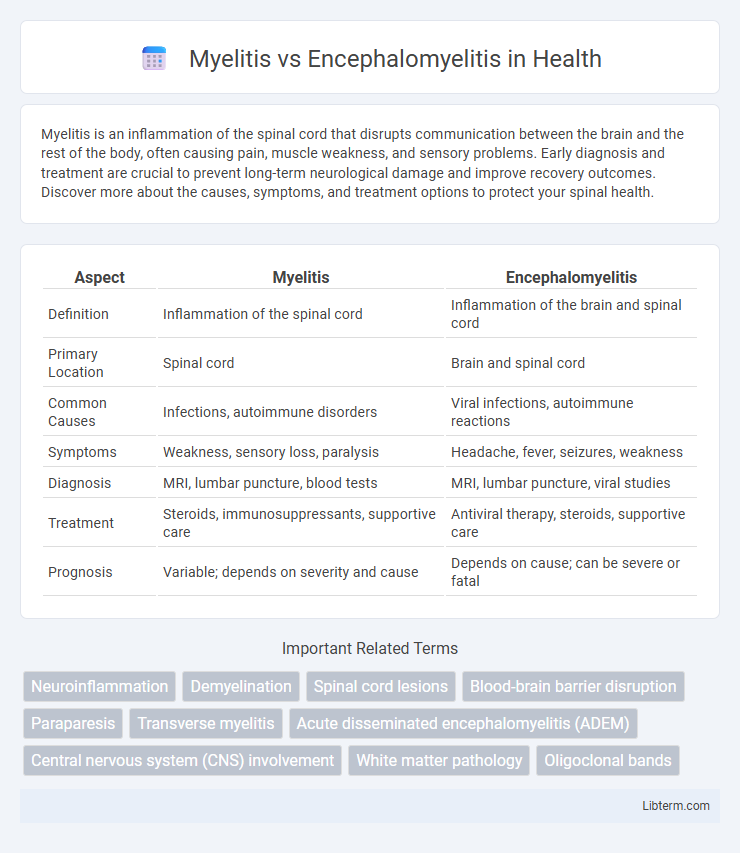
Myelitis is an inflammation of the spinal cord that disrupts communication between the brain and the rest of the body, often causing pain, muscle weakness, and sensory problems. Early diagnosis and treatment are crucial to prevent long-term neurological damage and improve recovery outcomes. Discover more about the causes, symptoms, and treatment options to protect your spinal health.
Table of Comparison
| Aspect | Myelitis | Encephalomyelitis |
|---|---|---|
| Definition | Inflammation of the spinal cord | Inflammation of the brain and spinal cord |
| Primary Location | Spinal cord | Brain and spinal cord |
| Common Causes | Infections, autoimmune disorders | Viral infections, autoimmune reactions |
| Symptoms | Weakness, sensory loss, paralysis | Headache, fever, seizures, weakness |
| Diagnosis | MRI, lumbar puncture, blood tests | MRI, lumbar puncture, viral studies |
| Treatment | Steroids, immunosuppressants, supportive care | Antiviral therapy, steroids, supportive care |
| Prognosis | Variable; depends on severity and cause | Depends on cause; can be severe or fatal |
Introduction to Myelitis and Encephalomyelitis
Myelitis refers to inflammation of the spinal cord, often caused by infections, autoimmune disorders, or traumatic injury, leading to symptoms such as muscle weakness, sensory disturbances, and paralysis. Encephalomyelitis involves inflammation of both the brain (encephalo-) and spinal cord (myelitis), typically presenting with more widespread neurological deficits including cognitive impairment, seizures, and motor dysfunction. Distinguishing between myelitis and encephalomyelitis is crucial for accurate diagnosis and targeted treatment strategies in neurological care.
Definitions: Myelitis vs Encephalomyelitis
Myelitis is inflammation confined to the spinal cord, often caused by infections, autoimmune disorders, or traumatic injury, leading to symptoms such as muscle weakness, sensory disturbances, and paralysis. Encephalomyelitis involves inflammation of both the brain (encephalo-) and spinal cord (myelitis), representing a more widespread central nervous system condition commonly triggered by viral infections or immune-mediated processes. Distinguishing between myelitis and encephalomyelitis is critical for diagnosis and treatment, as encephalomyelitis typically presents with broader neurological deficits including cognitive impairment and altered consciousness.
Causes and Risk Factors
Myelitis primarily results from viral infections such as herpes simplex virus or autoimmune disorders targeting the spinal cord, while encephalomyelitis involves inflammation of both the brain and spinal cord often triggered by viral infections like measles or autoimmune reactions. Risk factors for Myelitis include recent infections, autoimmune diseases, and exposure to toxins, whereas encephalomyelitis risk factors encompass prior viral illnesses, vaccination history, and genetic predispositions to immune system dysregulation. Understanding these distinct etiologies and risk profiles is crucial for accurate diagnosis and targeted treatment of these neuroinflammatory conditions.
Symptoms: Key Differences and Similarities
Myelitis primarily causes symptoms such as limb weakness, sensory disturbances, and bladder dysfunction due to inflammation of the spinal cord, while encephalomyelitis involves both the brain and spinal cord, leading to a combination of neurological deficits including cognitive impairment, seizures, and motor dysfunction. Both conditions share symptoms like muscle weakness and sensory loss, but encephalomyelitis often presents with more severe systemic neurological signs reflecting brain involvement. Accurate differentiation through MRI and cerebrospinal fluid analysis is critical for targeted treatment strategies in myelitis and encephalomyelitis.
Diagnostic Approaches
Magnetic resonance imaging (MRI) is the primary diagnostic tool to differentiate myelitis from encephalomyelitis, revealing inflammation confined to the spinal cord in myelitis versus combined brain and spinal cord lesions in encephalomyelitis. Cerebrospinal fluid (CSF) analysis typically shows pleocytosis and elevated protein in both conditions but may demonstrate distinct biomarker patterns such as oligoclonal bands more frequently in encephalomyelitis. Electrophysiological studies and serological tests aid in identifying underlying autoimmune or infectious etiologies, guiding accurate diagnosis and targeted treatment strategies.
Imaging and Laboratory Findings
Magnetic resonance imaging (MRI) of myelitis typically reveals spinal cord inflammation with hyperintense T2 lesions, often localized and segmental, whereas encephalomyelitis shows both brain and spinal cord involvement with diffuse or multifocal lesions. Cerebrospinal fluid (CSF) analysis in myelitis frequently demonstrates pleocytosis and elevated protein, while encephalomyelitis may present with similar CSF changes plus evidence of neuronal autoimmunity or viral markers. Differentiating these conditions relies on combining MRI patterns and CSF biomarkers to guide diagnosis and treatment strategies.
Treatment Options for Myelitis
Treatment options for myelitis primarily include high-dose corticosteroids to reduce spinal cord inflammation and plasma exchange therapy for severe or steroid-resistant cases. Immunosuppressive drugs like cyclophosphamide or azathioprine are considered when autoimmune causes are suspected. Supportive care involving physical therapy and pain management is crucial for recovery and symptom relief.
Management Strategies for Encephalomyelitis
Encephalomyelitis management primarily involves high-dose intravenous corticosteroids to reduce inflammation, often followed by immunosuppressive therapies such as plasma exchange or intravenous immunoglobulin in refractory cases. Supportive care includes symptom-specific treatments like antiepileptic drugs for seizures and physical rehabilitation to address motor deficits. Early diagnosis and aggressive treatment are crucial to improving neurological outcomes compared to isolated myelitis, which may require less intensive immunomodulatory approaches.
Prognosis and Long-term Outcomes
Myelitis typically involves inflammation of the spinal cord, presenting risks such as partial paralysis and sensory deficits, with prognosis varying based on severity and treatment timing, often leading to substantial functional recovery within months. Encephalomyelitis, affecting both the brain and spinal cord, is associated with more complex neurological impairments including cognitive dysfunction and motor deficits, resulting in a more prolonged recovery period and a higher likelihood of persistent neurological sequelae. Long-term outcomes differ significantly, with myelitis patients often regaining significant independence, whereas encephalomyelitis cases require ongoing rehabilitation due to extensive CNS involvement and risk of chronic disability.
Prevention and Patient Support
Preventing myelitis and encephalomyelitis involves vaccination against causative infections like measles, mumps, rubella, and influenza, alongside early treatment of viral or bacterial infections to reduce inflammation risk. Patient support includes comprehensive neurological assessments, physical therapy to maintain motor function, and psychological counseling to address cognitive or emotional challenges associated with these central nervous system inflammations. Immunomodulatory therapies, such as corticosteroids or plasma exchange, play a critical role in managing symptoms and improving long-term outcomes for affected individuals.
Myelitis Infographic
 libterm.com
libterm.com