Allodynia refers to a condition where normally non-painful stimuli, such as light touch or mild temperature changes, cause significant pain due to sensory nerve dysfunction. This symptom is commonly associated with disorders like fibromyalgia, neuropathy, and migraine, impacting quality of life by intensifying everyday sensations. Discover more about the causes, diagnosis, and treatment options to better manage your allodynia in the rest of the article.
Table of Comparison
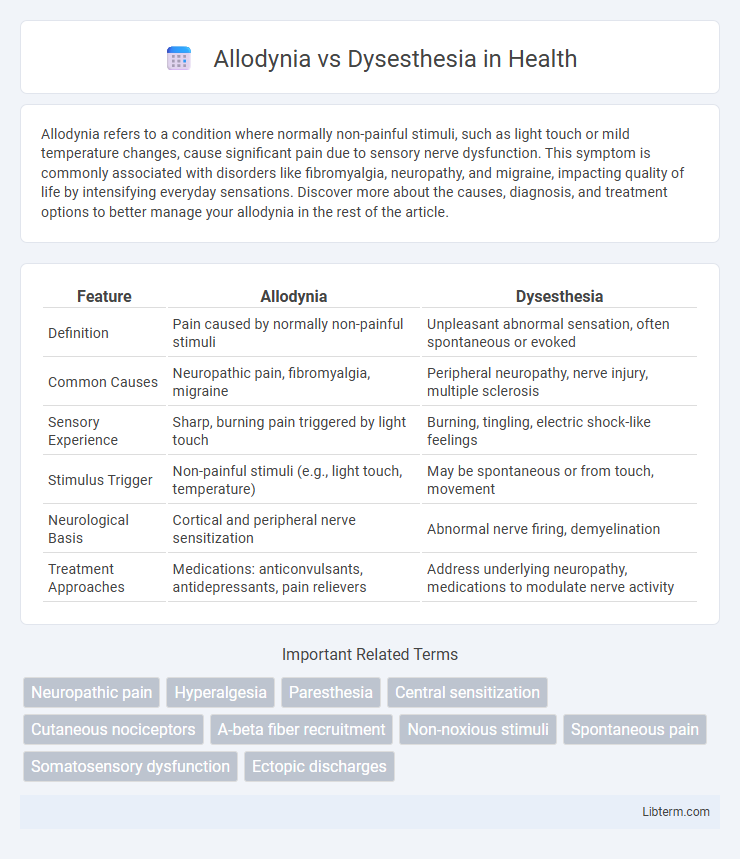
| Feature | Allodynia | Dysesthesia |
|---|---|---|
| Definition | Pain caused by normally non-painful stimuli | Unpleasant abnormal sensation, often spontaneous or evoked |
| Common Causes | Neuropathic pain, fibromyalgia, migraine | Peripheral neuropathy, nerve injury, multiple sclerosis |
| Sensory Experience | Sharp, burning pain triggered by light touch | Burning, tingling, electric shock-like feelings |
| Stimulus Trigger | Non-painful stimuli (e.g., light touch, temperature) | May be spontaneous or from touch, movement |
| Neurological Basis | Cortical and peripheral nerve sensitization | Abnormal nerve firing, demyelination |
| Treatment Approaches | Medications: anticonvulsants, antidepressants, pain relievers | Address underlying neuropathy, medications to modulate nerve activity |
Understanding Allodynia: Definition and Types
Allodynia is a pain disorder where normally non-painful stimuli, such as light touch or temperature changes, trigger discomfort, classified into tactile, thermal, and mechanical types. Tactile allodynia involves pain from light touch, thermal allodynia results from temperature differences, and mechanical allodynia arises from pressure or movement. Differentiating allodynia from dysesthesia, which involves unpleasant abnormal sensations regardless of stimuli, is critical for accurate diagnosis and treatment in neuropathic pain conditions.
What is Dysesthesia? Overview and Classification
Dysesthesia is a distressing abnormal sensation often described as burning, electric, or itching, resulting from nerve damage or dysfunction. It is classified into different types, including superficial dysesthesia, which affects the skin's surface, and deep dysesthesia, involving sensations within muscles or joints. Understanding these classifications aids in diagnosing neurological disorders and tailoring appropriate pain management strategies.
Key Differences: Allodynia vs Dysesthesia
Allodynia is a condition where normally non-painful stimuli, such as light touch or temperature, cause pain, whereas dysesthesia refers to unpleasant, abnormal sensations that can be painful, burning, or tingling without an external stimulus. The key difference lies in allodynia involving pain triggered by external, non-painful stimuli, while dysesthesia encompasses spontaneous or stimulus-evoked abnormal sensations that are not limited to pain. Understanding these distinctions is crucial for accurate diagnosis and targeted treatment in neuropathic pain management.
Common Causes of Allodynia
Allodynia often results from nerve damage or conditions like neuropathy, fibromyalgia, and postherpetic neuralgia, where normally non-painful stimuli trigger pain responses. Dysesthesia, by contrast, involves abnormal sensations such as burning or tingling, typically linked to nerve injury or neurological disorders. Understanding the common causes of allodynia, including peripheral nerve injury, central sensitization, and inflammatory processes, is crucial for accurate diagnosis and targeted treatment.
Typical Causes of Dysesthesia
Dysesthesia is often caused by nerve damage or dysfunction resulting from conditions such as diabetic neuropathy, multiple sclerosis, or postherpetic neuralgia. Unlike allodynia, which is pain due to normally non-painful stimuli, dysesthesia involves unpleasant abnormal sensations, including burning, itching, or electric shock-like feelings. Central or peripheral nervous system injuries and chemotherapy-induced neuropathy are also common contributors to dysesthesia development.
Symptoms and Sensory Experiences
Allodynia presents as pain from stimuli that normally do not cause pain, such as light touch or gentle pressure, often described as burning, aching, or stabbing sensations. Dysesthesia involves abnormal, unpleasant sensations that may be spontaneous or evoked, including burning, electric shocks, or crawling feelings on the skin. Both conditions reflect altered sensory processing but differ in triggers, with allodynia being sensitivity to non-painful stimuli and dysesthesia encompassing a broader range of discomfort, including spontaneous sensations.
Diagnostic Methods for Sensory Disorders
Diagnostic methods for allodynia and dysesthesia primarily involve detailed clinical evaluations using quantitative sensory testing (QST) to assess abnormal pain responses and sensory abnormalities. Neurophysiological assessments, such as nerve conduction studies and somatosensory evoked potentials, help differentiate peripheral or central nervous system involvement in these sensory disorders. Advanced imaging techniques like functional MRI provide further insights into altered brain activity patterns associated with these conditions.
Treatment Options for Allodynia
Treatment options for allodynia primarily include medications such as anticonvulsants like gabapentin and pregabalin, which help stabilize nerve signals and reduce pain sensitivity. Topical agents such as lidocaine patches or capsaicin cream provide localized relief by numbing affected areas or desensitizing nerve endings. Physical therapy and cognitive-behavioral therapy may complement pharmacological approaches by improving nerve function and managing pain perception in patients with allodynia.
Management Strategies for Dysesthesia
Management strategies for dysesthesia primarily include pharmacological treatments such as anticonvulsants (gabapentin, pregabalin) and antidepressants (duloxetine, amitriptyline) to modulate nerve pain signals. Non-pharmacological approaches like physical therapy, cognitive-behavioral therapy, and transcutaneous electrical nerve stimulation (TENS) are effective in reducing symptoms and improving quality of life. Early diagnosis and a multidisciplinary approach optimize outcomes by addressing the underlying nerve dysfunction and associated neuropathic pain.
Living with Chronic Sensory Dysfunction
Living with chronic sensory dysfunction such as allodynia and dysesthesia involves managing abnormal pain sensations triggered by stimuli that typically cause no discomfort or by spontaneous sensations. Allodynia causes pain from normally non-painful stimuli like light touch, while dysesthesia involves unpleasant, abnormal sensations that can occur without an external trigger. Effective management often includes multidisciplinary approaches combining medication, physical therapy, and psychological support to improve quality of life and reduce symptom severity.
Allodynia Infographic
 libterm.com
libterm.com