Polyarthritis involves inflammation in five or more joints, causing pain, stiffness, and swelling that may affect your mobility and daily activities. Common causes include rheumatoid arthritis, lupus, and infections, with symptoms requiring timely diagnosis and treatment to prevent joint damage. Explore this article to understand polyarthritis causes, symptoms, and effective management strategies tailored to your needs.
Table of Comparison
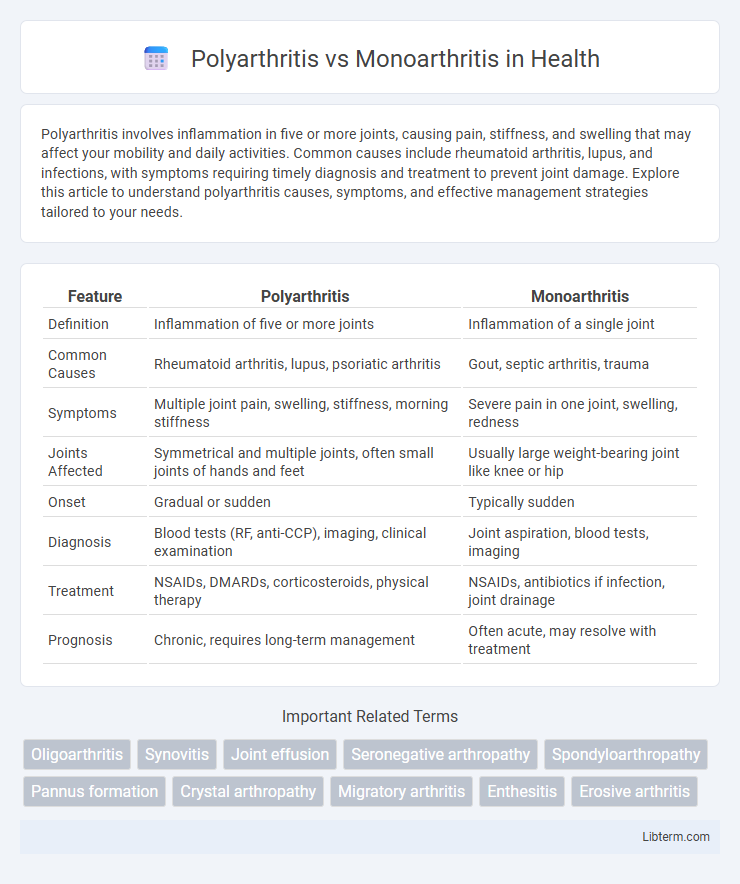
| Feature | Polyarthritis | Monoarthritis |
|---|---|---|
| Definition | Inflammation of five or more joints | Inflammation of a single joint |
| Common Causes | Rheumatoid arthritis, lupus, psoriatic arthritis | Gout, septic arthritis, trauma |
| Symptoms | Multiple joint pain, swelling, stiffness, morning stiffness | Severe pain in one joint, swelling, redness |
| Joints Affected | Symmetrical and multiple joints, often small joints of hands and feet | Usually large weight-bearing joint like knee or hip |
| Onset | Gradual or sudden | Typically sudden |
| Diagnosis | Blood tests (RF, anti-CCP), imaging, clinical examination | Joint aspiration, blood tests, imaging |
| Treatment | NSAIDs, DMARDs, corticosteroids, physical therapy | NSAIDs, antibiotics if infection, joint drainage |
| Prognosis | Chronic, requires long-term management | Often acute, may resolve with treatment |
Introduction to Polyarthritis and Monoarthritis
Polyarthritis involves inflammation affecting five or more joints simultaneously, often linked to autoimmune conditions such as rheumatoid arthritis or viral infections. Monoarthritis refers to inflammation restricted to a single joint, commonly caused by trauma, gout, or septic arthritis. Differentiating between polyarthritis and monoarthritis is crucial for diagnosis and guiding appropriate treatment strategies.
Defining Polyarthritis: Key Characteristics
Polyarthritis is characterized by inflammation affecting five or more joints simultaneously, contrasting with monoarthritis, which involves only one joint. This condition often signals systemic diseases such as rheumatoid arthritis or lupus, leading to symmetrical joint swelling, pain, and stiffness. Early diagnosis through clinical examination and imaging is crucial for managing polyarthritis effectively and preventing joint damage.
Understanding Monoarthritis: Main Features
Monoarthritis involves inflammation in a single joint, typically presenting with sudden onset of pain, swelling, and limited range of motion. It is often caused by infections, crystal-induced arthritis like gout, or traumatic injury, distinguishing it from polyarthritis which affects multiple joints simultaneously. Accurate diagnosis relies on clinical evaluation, joint fluid analysis, and imaging to identify the specific etiology and guide targeted treatment.
Common Causes of Polyarthritis
Polyarthritis commonly results from autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus, where multiple joints become inflamed simultaneously. Infectious causes like viral arthritis from parvovirus B19 and bacterial infections also contribute to polyarthritis development. Unlike monoarthritis, which affects a single joint often due to trauma or gout, polyarthritis involves widespread joint inflammation requiring distinct diagnostic and therapeutic approaches.
Common Causes of Monoarthritis
Monoarthritis typically results from infections such as septic arthritis caused by bacteria like Staphylococcus aureus, gout characterized by uric acid crystal deposition, or trauma leading to joint inflammation. Common causes also include Lyme disease and pseudogout, where calcium pyrophosphate crystals accumulate in the joint. Differentiating monoarthritis from polyarthritis, which involves multiple joints, is crucial for accurate diagnosis and targeted treatment strategies.
Symptom Comparison: Polyarthritis vs Monoarthritis
Polyarthritis involves inflammation affecting five or more joints simultaneously, often causing widespread pain, swelling, and stiffness, whereas monoarthritis targets a single joint with intense pain, swelling, and restricted movement. Polyarthritis symptoms typically present symmetrically in multiple joints such as hands, knees, and wrists, while monoarthritis usually manifests acutely in one joint, commonly the knee or hip. Systemic symptoms like fever and fatigue are more common in polyarthritis due to underlying autoimmune or infectious causes, while monoarthritis often results from localized infection or trauma.
Diagnostic Approaches for Polyarthritis and Monoarthritis
Diagnosing polyarthritis involves comprehensive clinical evaluation, including detailed patient history, physical examination of multiple joints, and laboratory tests such as rheumatoid factor, anti-CCP antibodies, and ESR or CRP to assess systemic inflammation. Monoarthritis diagnosis prioritizes synovial fluid analysis from the affected joint to detect infection, crystals, or inflammatory markers, supplemented by imaging techniques like X-rays or ultrasound to identify joint damage or effusion. Both conditions require targeted diagnostic approaches to differentiate underlying causes such as autoimmune diseases in polyarthritis or septic arthritis, gout, or trauma in monoarthritis.
Treatment Options: Polyarthritis vs Monoarthritis
Treatment options for polyarthritis typically involve systemic therapies such as disease-modifying antirheumatic drugs (DMARDs), biologics, and corticosteroids to control widespread joint inflammation and prevent joint damage. In contrast, monoarthritis treatment often targets the underlying cause, such as antibiotics for septic arthritis, nonsteroidal anti-inflammatory drugs (NSAIDs) for gout, or joint aspiration combined with corticosteroid injections for inflammatory flare-ups. Early diagnosis and tailored treatment strategies are essential in both conditions to minimize joint destruction and improve patient quality of life.
Prognosis and Long-Term Outcomes
Polyarthritis often indicates a systemic inflammatory condition, such as rheumatoid arthritis, with a prognosis that may involve chronic joint damage and disability if untreated, whereas monoarthritis usually suggests localized issues like gout or infection, potentially resolving with targeted therapy. Long-term outcomes in polyarthritis depend on early diagnosis and aggressive management to prevent joint erosion, while monoarthritis prognosis improves with prompt identification and treatment of the underlying cause, minimizing the risk of recurrent episodes. Monitoring disease progression through imaging and serological markers is crucial for optimizing therapeutic strategies in both conditions.
Polyarthritis vs Monoarthritis: Which One Needs Urgent Attention?
Polyarthritis involves inflammation in five or more joints, often indicating systemic diseases like rheumatoid arthritis, which requires urgent medical evaluation due to its potential for rapid joint damage. Monoarthritis affects a single joint and is commonly caused by infections, gout, or trauma, making urgent attention necessary when infection or septic arthritis is suspected to prevent severe complications. Timely diagnosis and treatment are critical in both conditions, but polyarthritis often signals widespread inflammation demanding comprehensive management.
Polyarthritis Infographic
 libterm.com
libterm.com