Meningitis is a serious infection causing inflammation of the protective membranes covering the brain and spinal cord, often resulting from bacterial or viral causes. Early symptoms include fever, headache, and neck stiffness, and prompt diagnosis and treatment are critical to prevent severe complications or death. Learn more about the causes, symptoms, and treatment options to protect your health in the full article.
Table of Comparison
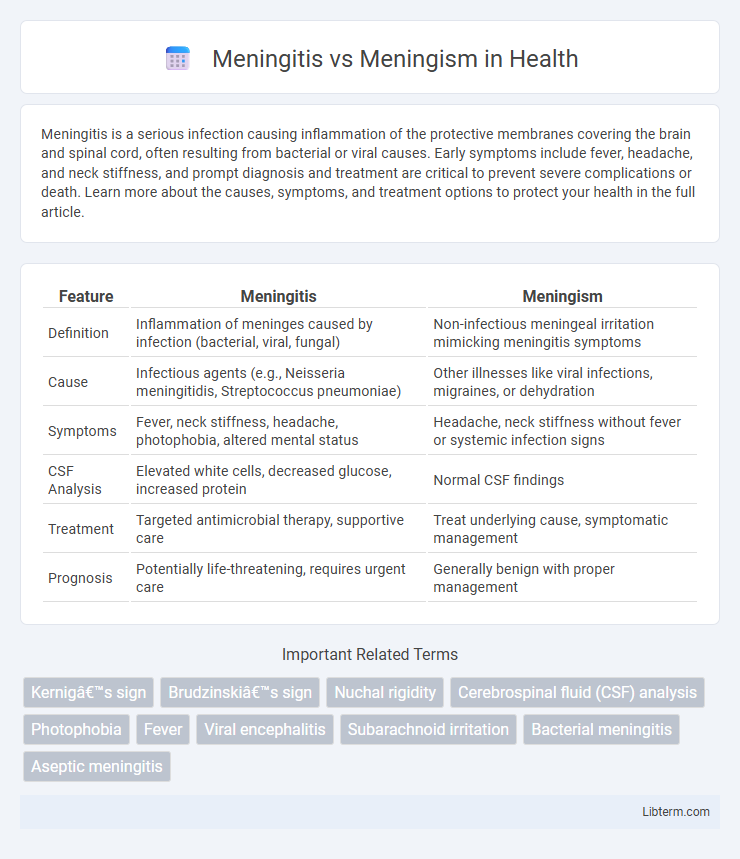
| Feature | Meningitis | Meningism |
|---|---|---|
| Definition | Inflammation of meninges caused by infection (bacterial, viral, fungal) | Non-infectious meningeal irritation mimicking meningitis symptoms |
| Cause | Infectious agents (e.g., Neisseria meningitidis, Streptococcus pneumoniae) | Other illnesses like viral infections, migraines, or dehydration |
| Symptoms | Fever, neck stiffness, headache, photophobia, altered mental status | Headache, neck stiffness without fever or systemic infection signs |
| CSF Analysis | Elevated white cells, decreased glucose, increased protein | Normal CSF findings |
| Treatment | Targeted antimicrobial therapy, supportive care | Treat underlying cause, symptomatic management |
| Prognosis | Potentially life-threatening, requires urgent care | Generally benign with proper management |
Understanding Meningitis: Definition and Overview
Meningitis is the inflammation of the protective membranes covering the brain and spinal cord, primarily caused by bacterial, viral, or fungal infections, leading to symptoms such as fever, headache, neck stiffness, and altered mental status. It requires prompt diagnosis and treatment to prevent severe complications like brain damage, hearing loss, or death. Understanding meningitis involves recognizing its infectious etiology and differentiating it from meningism, a condition presenting with similar symptoms but without actual infection or inflammation of the meninges.
What Is Meningism? Key Features and Meaning
Meningism refers to a clinical syndrome characterized by symptoms resembling meningitis without actual inflammation of the meninges, typically caused by non-infectious conditions such as viral infections, migraines, or subarachnoid hemorrhage. Key features include neck stiffness, photophobia, and headache, but cerebrospinal fluid (CSF) analysis remains normal, distinguishing it from true meningitis. Understanding meningism is crucial for accurate diagnosis and avoiding unnecessary antibiotic treatment in patients presenting with meningeal irritation signs.
Meningitis vs Meningism: Core Differences
Meningitis involves inflammation of the meninges caused by infection, presenting with fever, neck stiffness, and altered mental status, whereas meningism mimics meningitis symptoms like neck stiffness and headache without actual meningeal inflammation or infection. Meningism often arises from systemic illnesses such as viral infections, dehydration, or metabolic disturbances, making cerebrospinal fluid (CSF) analysis normal compared to the abnormal CSF findings in meningitis. Differentiating these conditions is critical for appropriate treatment, as meningitis requires urgent antimicrobial therapy, while meningism typically resolves with supportive care.
Causes of Meningitis: Infections and Risk Factors
Meningitis is primarily caused by infections from bacteria such as Neisseria meningitidis and Streptococcus pneumoniae, viruses including enteroviruses, and, less commonly, fungi or parasites. Risk factors increasing susceptibility to meningitis include age extremes (infants and elderly), immunocompromised states, close living conditions (e.g., dormitories), and recent head trauma or neurosurgery. Differentiating meningitis from meningism, which mimics meningitis symptoms without infection, relies heavily on identifying the infectious etiology and associated risk factors.
Causes of Meningism: Underlying Triggers
Meningism is characterized by symptoms mimicking meningitis, including headache, neck stiffness, and photophobia, but without actual inflammation of the meninges. Causes of meningism primarily include viral infections such as influenza and enteroviruses, as well as non-infectious triggers like subarachnoid hemorrhage, migraines, and medication side effects, which irritate the meninges without causing infection. Distinguishing these underlying triggers is crucial for accurate diagnosis and appropriate management, avoiding unnecessary antimicrobial treatments.
Signs and Symptoms: Comparing Clinical Presentations
Meningitis presents with signs such as high fever, severe headache, neck stiffness, photophobia, and altered mental status, reflecting inflammation of the meninges usually caused by infection. Meningism mimics meningitis but lacks bacterial or viral infection evidence, with symptoms like headache, neck stiffness, and photophobia typically due to non-infectious causes such as migraine or subarachnoid hemorrhage. Differentiating these conditions relies on clinical features including absence of systemic infection signs in meningism and cerebrospinal fluid analysis revealing pleocytosis in meningitis.
Diagnostic Approaches: Meningitis vs Meningism
Diagnostic approaches for meningitis emphasize cerebrospinal fluid (CSF) analysis through lumbar puncture, revealing elevated white blood cell count, decreased glucose, and increased protein levels indicative of infection. In contrast, meningism, characterized by symptoms mimicking meningitis without infection, presents normal CSF findings, often requiring clinical assessment and exclusion of infectious causes. Neuroimaging and blood cultures further aid differentiation, ensuring accurate diagnosis and appropriate treatment strategies.
Treatment Options for Meningitis
Treatment options for meningitis primarily depend on its cause, with bacterial meningitis requiring immediate intravenous antibiotics such as ceftriaxone or vancomycin to reduce mortality and complications. Viral meningitis generally necessitates supportive care, including fluids, rest, and pain relief, as most viral cases resolve without specific antiviral treatment except for herpes simplex virus infections treated with acyclovir. Corticosteroids may be administered in bacterial meningitis to reduce inflammation and neurological damage, while meningism, a non-infectious condition presenting with meningitis-like symptoms, typically resolves without targeted treatment once the underlying cause, such as migraine or medication side effects, is addressed.
Management and Care for Meningism
Management of meningism primarily involves symptomatic care, as it mimics meningitis without actual infection. Key interventions include pain relief using analgesics and hydration to address headache and fever symptoms. Unlike meningitis, meningism does not require antibiotics or hospital admission, emphasizing careful monitoring and reassurance to prevent unnecessary invasive treatment.
Prevention Strategies and Prognosis Comparison
Meningitis prevention involves vaccination against common pathogens like Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b, along with maintaining good hygiene and prompt treatment of infections to reduce morbidity and mortality. Meningism, characterized by meningeal irritation symptoms without infection, requires addressing underlying causes such as viral illnesses or medications, with no specific vaccine but emphasis on symptom management to prevent progression. Prognosis for meningitis varies widely based on etiology and timely intervention, with bacterial meningitis posing higher risks of complications and mortality compared to meningism, which generally has a benign and self-limiting course.
Meningitis Infographic
 libterm.com
libterm.com