Fibrosis is the excessive formation of connective tissue in an organ or tissue, often resulting from chronic inflammation or injury. This process can impair normal function by replacing healthy cells with scar tissue, leading to complications in organs such as the lungs, liver, or heart. Explore the rest of this article to understand how fibrosis develops and what measures can help manage its impact on your health.
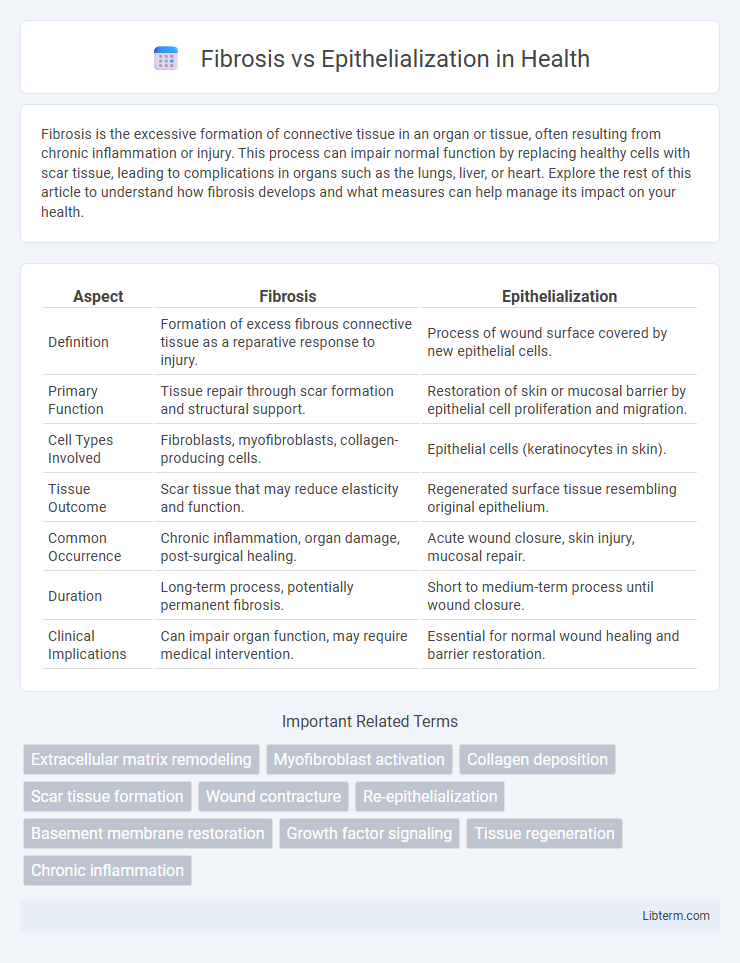
Table of Comparison
| Aspect | Fibrosis | Epithelialization |
|---|---|---|
| Definition | Formation of excess fibrous connective tissue as a reparative response to injury. | Process of wound surface covered by new epithelial cells. |
| Primary Function | Tissue repair through scar formation and structural support. | Restoration of skin or mucosal barrier by epithelial cell proliferation and migration. |
| Cell Types Involved | Fibroblasts, myofibroblasts, collagen-producing cells. | Epithelial cells (keratinocytes in skin). |
| Tissue Outcome | Scar tissue that may reduce elasticity and function. | Regenerated surface tissue resembling original epithelium. |
| Common Occurrence | Chronic inflammation, organ damage, post-surgical healing. | Acute wound closure, skin injury, mucosal repair. |
| Duration | Long-term process, potentially permanent fibrosis. | Short to medium-term process until wound closure. |
| Clinical Implications | Can impair organ function, may require medical intervention. | Essential for normal wound healing and barrier restoration. |
Understanding Fibrosis and Epithelialization
Fibrosis is the pathological accumulation of excess fibrous connective tissue during wound healing, often leading to tissue scarring and impaired organ function. Epithelialization is the biological process where epithelial cells migrate, proliferate, and cover a wound, restoring the skin barrier and tissue integrity. Understanding the balance between fibrosis and epithelialization is crucial for developing therapies that promote effective healing while minimizing scar formation.
Key Differences Between Fibrosis and Epithelialization
Fibrosis involves the excessive accumulation of extracellular matrix proteins leading to scar tissue formation, often impairing normal tissue function, whereas epithelialization is the process where epithelial cells migrate, proliferate, and cover a wound to restore the skin barrier. Key differences include fibrosis resulting in dense, fibrotic tissue disrupting organ architecture, while epithelialization promotes tissue regeneration and surface repair without scar formation. Fibrosis typically follows chronic injury or inflammation, whereas epithelialization predominantly occurs during the proliferative phase of acute wound healing.
The Biological Mechanisms of Fibrosis
Fibrosis arises from the excessive accumulation of extracellular matrix components, primarily collagen, driven by the persistent activation of fibroblasts and myofibroblasts in response to chronic tissue injury. Key biological mechanisms involve the release of pro-fibrotic cytokines such as transforming growth factor-beta (TGF-b), which promotes fibroblast proliferation, differentiation, and reduced matrix degradation. In contrast to epithelialization, which restores tissue integrity through the migration and proliferation of epithelial cells, fibrosis results in pathological scarring that impairs normal tissue architecture and function.
Epithelialization: Steps and Significance
Epithelialization is a crucial phase in wound healing where epithelial cells migrate, proliferate, and differentiate to cover the wound bed, restoring the barrier function of the skin. The process involves the activation of basal keratinocytes, their migration over the granulation tissue, and subsequent stratification to form a new epithelial layer. This restoration minimizes infection risk, prevents fluid loss, and is essential for functional tissue repair, contrasting with fibrosis, which leads to scar formation and potential tissue dysfunction.
Roles in Wound Healing: Fibrosis vs Epithelialization
Fibrosis involves the excessive deposition of extracellular matrix components by fibroblasts, leading to scar tissue formation that restores tissue integrity but may impair function. Epithelialization is the process where epithelial cells migrate, proliferate, and differentiate to cover the wound surface, re-establishing the protective barrier of skin or mucosa. Both processes are critical in wound healing; fibrosis provides structural support while epithelialization ensures barrier restoration.
Factors Influencing Fibrosis and Epithelialization
Factors influencing fibrosis include chronic inflammation, persistent tissue injury, and dysregulated wound healing processes characterized by excess fibroblast activation and extracellular matrix deposition. Epithelialization is promoted by adequate oxygenation, growth factors such as EGF and TGF-a, and intact basal membrane structures facilitating keratinocyte migration and proliferation. Balancing pro-fibrotic cytokines like TGF-b and anti-fibrotic mechanisms is crucial for directing repair toward epithelial regeneration instead of fibrotic scar formation.
Clinical Implications of Excessive Fibrosis
Excessive fibrosis leads to the formation of dense scar tissue, impairing normal tissue architecture and function, which can result in chronic organ dysfunction and reduced regenerative capacity. In contrast, epithelialization restores the integrity of the mucosal or skin surface by promoting the migration and proliferation of epithelial cells, critical for wound healing and barrier protection. Clinical implications of excessive fibrosis include increased risk of organ failure, persistent inflammation, and complications such as contractures or adhesions that may necessitate surgical intervention.
Promoting Effective Epithelialization in Healing
Promoting effective epithelialization accelerates wound closure by encouraging keratinocyte migration and proliferation, which restores the skin barrier and reduces infection risk. Fibrosis, characterized by excessive fibroblast activity and collagen deposition, can impede epithelialization and lead to scar formation rather than functional tissue regeneration. Optimizing growth factors like EGF and TGF-b modulation improves epithelial cell function, minimizing fibrosis and supporting regenerative healing.
Therapeutic Approaches: Reducing Fibrosis, Enhancing Epithelialization
Therapeutic approaches targeting fibrosis focus on antifibrotic agents such as pirfenidone and nintedanib, which inhibit fibroblast activation and collagen deposition to reduce tissue scarring. Enhancing epithelialization involves the application of growth factors like epidermal growth factor (EGF) and keratinocyte growth factor (KGF), which promote keratinocyte proliferation and migration, accelerating wound closure. Biomaterial scaffolds combined with stem cell therapy are emerging as advanced strategies to simultaneously suppress fibrosis and stimulate epithelial tissue regeneration.
Future Directions in Fibrosis and Epithelialization Research
Future directions in fibrosis and epithelialization research emphasize developing targeted molecular therapies to modulate fibroblast activity and enhance epithelial regeneration. Advances in gene editing techniques such as CRISPR-Cas9 hold promise for correcting genetic aberrations contributing to pathological fibrosis and impaired wound healing. Integration of biomaterials and stem cell technology aims to create innovative regenerative treatments that balance fibrosis prevention with effective epithelialization, improving outcomes in chronic wound management and organ fibrosis.
Fibrosis Infographic
 libterm.com
libterm.com