Hepatitis is an inflammation of the liver that can result from viral infections, alcohol use, or autoimmune diseases, leading to symptoms like jaundice, fatigue, and abdominal pain. Early diagnosis and proper treatment are essential to prevent serious complications such as liver cirrhosis or cancer. Explore the rest of this article to understand causes, symptoms, and effective management strategies for hepatitis.
Table of Comparison
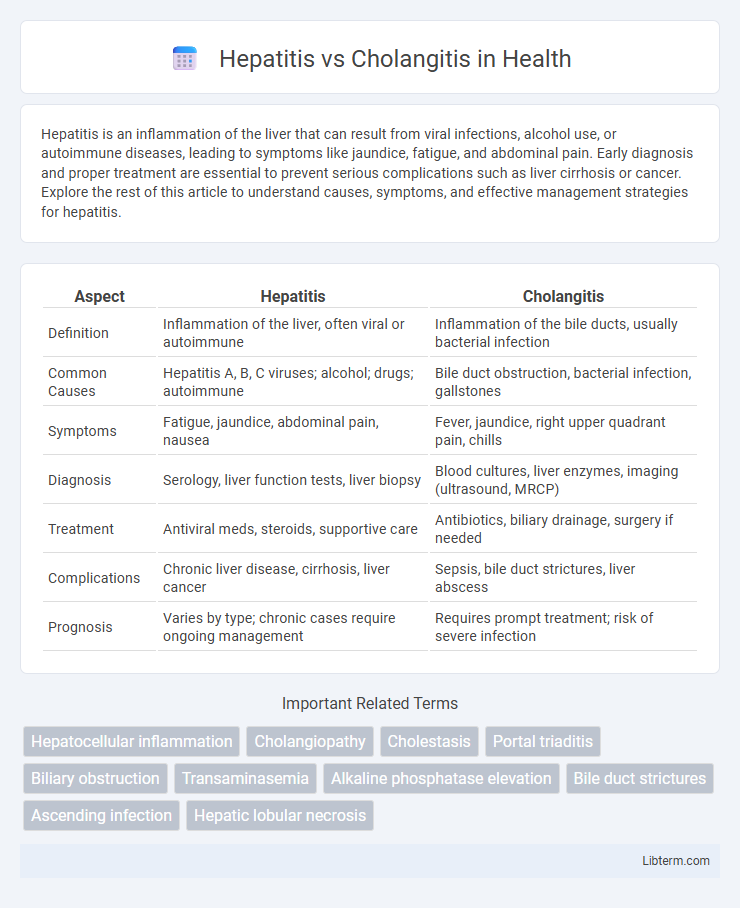
| Aspect | Hepatitis | Cholangitis |
|---|---|---|
| Definition | Inflammation of the liver, often viral or autoimmune | Inflammation of the bile ducts, usually bacterial infection |
| Common Causes | Hepatitis A, B, C viruses; alcohol; drugs; autoimmune | Bile duct obstruction, bacterial infection, gallstones |
| Symptoms | Fatigue, jaundice, abdominal pain, nausea | Fever, jaundice, right upper quadrant pain, chills |
| Diagnosis | Serology, liver function tests, liver biopsy | Blood cultures, liver enzymes, imaging (ultrasound, MRCP) |
| Treatment | Antiviral meds, steroids, supportive care | Antibiotics, biliary drainage, surgery if needed |
| Complications | Chronic liver disease, cirrhosis, liver cancer | Sepsis, bile duct strictures, liver abscess |
| Prognosis | Varies by type; chronic cases require ongoing management | Requires prompt treatment; risk of severe infection |
Introduction to Hepatitis and Cholangitis
Hepatitis is an inflammation of the liver commonly caused by viral infections such as hepatitis A, B, C, D, and E, toxic substances, or autoimmune diseases. Cholangitis refers to inflammation of the bile ducts, often resulting from bacterial infection due to bile duct obstruction or strictures. Understanding the distinct pathophysiology and clinical presentations of hepatitis and cholangitis is essential for accurate diagnosis and targeted treatment.
Defining Hepatitis: Causes and Types
Hepatitis refers to inflammation of the liver caused by viral infections, autoimmune diseases, toxins, or alcohol abuse. Common types include Hepatitis A, B, C, D, and E, each varying in transmission mode and severity. Understanding the viral etiology and distinguishing between acute and chronic hepatitis is crucial for accurate diagnosis and treatment.
Understanding Cholangitis: Key Features
Cholangitis is an infection or inflammation of the bile ducts, often caused by bacterial obstruction such as gallstones or strictures, leading to symptoms like fever, jaundice, and right upper quadrant pain known as Charcot's triad. Unlike hepatitis, which primarily affects liver cells causing inflammation due to viral infections like hepatitis A, B, or C, cholangitis involves bile duct pathology and can rapidly progress to sepsis if untreated. Diagnosis relies on imaging techniques such as MRCP or ERCP and laboratory tests showing elevated bilirubin, alkaline phosphatase, and white blood cell count, necessitating prompt antibiotic therapy and sometimes endoscopic intervention.
Epidemiology and Risk Factors
Hepatitis predominantly affects populations exposed to viral infections such as Hepatitis A, B, C, D, and E, with risk factors including intravenous drug use, unprotected sexual contact, and contaminated food or water. Cholangitis is commonly linked to biliary obstruction caused by gallstones, strictures, or tumors, and occurs more frequently in older adults or individuals with underlying hepatobiliary diseases such as primary sclerosing cholangitis. Epidemiological studies indicate higher hepatitis prevalence in regions with poor sanitation and limited healthcare access, while cholangitis incidence correlates with conditions causing bile duct obstruction and cholestasis.
Clinical Presentation: Symptoms Comparison
Hepatitis typically presents with symptoms such as fatigue, jaundice, abdominal pain, nausea, and dark urine, reflecting liver inflammation. Cholangitis is characterized by the Charcot's triad: fever, right upper quadrant pain, and jaundice, indicating bile duct infection and obstruction. Fever and chills are more prominent in cholangitis, whereas hepatitis often includes systemic symptoms like malaise and anorexia.
Diagnostic Approaches for Hepatitis vs Cholangitis
Diagnostic approaches for hepatitis primarily involve serologic tests detecting viral antigens and antibodies, liver function tests showing elevated ALT and AST levels, and imaging studies like ultrasound to assess liver inflammation. In contrast, cholangitis diagnosis relies heavily on clinical presentation, elevated cholestatic liver enzymes such as alkaline phosphatase and bilirubin, blood cultures identifying infectious agents, and imaging techniques including MRCP or ERCP to visualize bile duct obstruction or inflammation. Differentiating these conditions involves combining laboratory data and imaging findings to target viral hepatitis versus biliary tract infection or obstruction characteristic of cholangitis.
Laboratory and Imaging Findings
Hepatitis typically shows elevated liver enzymes, specifically alanine aminotransferase (ALT) and aspartate aminotransferase (AST), often with a pronounced increase in ALT levels, along with abnormal bilirubin and alkaline phosphatase in severe cases. Cholangitis presents with elevated alkaline phosphatase and gamma-glutamyl transferase (GGT) due to bile duct inflammation or obstruction, frequently accompanied by leukocytosis and elevated C-reactive protein (CRP). Imaging findings in hepatitis are generally nonspecific but may show liver enlargement on ultrasound or MRI, whereas cholangitis is characterized by bile duct dilation, strictures, or stones visualized through ultrasound, magnetic resonance cholangiopancreatography (MRCP), or endoscopic retrograde cholangiopancreatography (ERCP).
Complications and Prognosis
Hepatitis complications include chronic liver disease, cirrhosis, and hepatocellular carcinoma, significantly impacting long-term prognosis. Cholangitis complications involve biliary sepsis, liver abscess, and secondary biliary cirrhosis, posing risks for severe infection and liver failure. Early diagnosis and treatment improve outcomes, but untreated cholangitis has a higher mortality rate due to infectious complications compared to most forms of hepatitis.
Treatment Strategies: Medical and Surgical Options
Hepatitis treatment strategies primarily involve antiviral medications for viral causes, immunosuppressive drugs for autoimmune hepatitis, and supportive care to manage symptoms and prevent liver damage. Cholangitis requires urgent antibiotic therapy to treat bacterial infection and may involve endoscopic retrograde cholangiopancreatography (ERCP) or surgical drainage to relieve bile duct obstruction. In severe cases of both conditions, liver transplantation may be considered when medical and minimally invasive approaches fail to restore hepatic function or biliary flow.
Prevention and Patient Education
Preventing hepatitis involves vaccination against hepatitis A and B viruses, practicing safe injection techniques, and avoiding contaminated food and water to reduce infection risks. For cholangitis, prompt treatment of bile duct obstructions and maintaining good hygiene during medical procedures can lower incidence rates. Patient education should emphasize recognizing early symptoms, adherence to prescribed treatments, and lifestyle modifications to support liver and biliary health.
Hepatitis Infographic
 libterm.com
libterm.com