Hyperhidrosis, characterized by excessive sweating, can often be a symptom linked to hyperthyroidism, a condition where the thyroid gland produces too much hormone, accelerating metabolism and triggering increased perspiration. Managing hyperthyroidism effectively may reduce the severity of hyperhidrosis, improving your comfort and quality of life. Explore the rest of this article to understand the connection between these conditions and the best approaches to diagnosis and treatment.
Table of Comparison
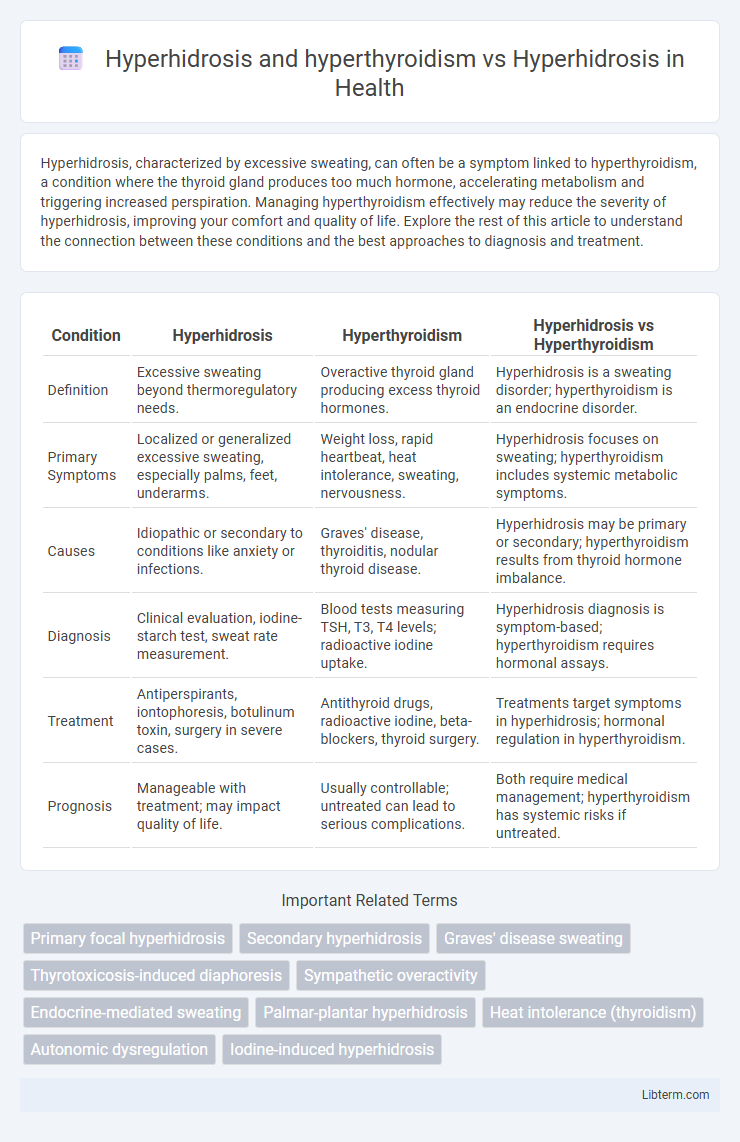
| Condition | Hyperhidrosis | Hyperthyroidism | Hyperhidrosis vs Hyperthyroidism |
|---|---|---|---|
| Definition | Excessive sweating beyond thermoregulatory needs. | Overactive thyroid gland producing excess thyroid hormones. | Hyperhidrosis is a sweating disorder; hyperthyroidism is an endocrine disorder. |
| Primary Symptoms | Localized or generalized excessive sweating, especially palms, feet, underarms. | Weight loss, rapid heartbeat, heat intolerance, sweating, nervousness. | Hyperhidrosis focuses on sweating; hyperthyroidism includes systemic metabolic symptoms. |
| Causes | Idiopathic or secondary to conditions like anxiety or infections. | Graves' disease, thyroiditis, nodular thyroid disease. | Hyperhidrosis may be primary or secondary; hyperthyroidism results from thyroid hormone imbalance. |
| Diagnosis | Clinical evaluation, iodine-starch test, sweat rate measurement. | Blood tests measuring TSH, T3, T4 levels; radioactive iodine uptake. | Hyperhidrosis diagnosis is symptom-based; hyperthyroidism requires hormonal assays. |
| Treatment | Antiperspirants, iontophoresis, botulinum toxin, surgery in severe cases. | Antithyroid drugs, radioactive iodine, beta-blockers, thyroid surgery. | Treatments target symptoms in hyperhidrosis; hormonal regulation in hyperthyroidism. |
| Prognosis | Manageable with treatment; may impact quality of life. | Usually controllable; untreated can lead to serious complications. | Both require medical management; hyperthyroidism has systemic risks if untreated. |
Understanding Hyperhidrosis: Definition and Types
Hyperhidrosis is a medical condition characterized by excessive sweating beyond what is necessary for temperature regulation, with primary hyperhidrosis stemming from overactive sweat glands and secondary hyperhidrosis resulting from underlying health issues like hyperthyroidism. Hyperthyroidism, an overactive thyroid gland producing excessive thyroid hormones, can induce secondary hyperhidrosis by accelerating metabolism and increasing body heat. Differentiating between primary hyperhidrosis and the hyperhidrosis caused by hyperthyroidism is crucial for targeted treatment and managing symptoms effectively.
What Is Hyperthyroidism? Key Features
Hyperthyroidism is a condition characterized by the overproduction of thyroid hormones, leading to an accelerated metabolism and symptoms such as weight loss, rapid heartbeat, and excessive sweating. Unlike hyperhidrosis, which specifically involves abnormal sweating often without an underlying systemic cause, hyperthyroidism-induced hyperhidrosis results from thyroid hormone imbalance. Key features of hyperthyroidism include heat intolerance, nervousness, tremors, and increased sweating, distinguishing it from primary hyperhidrosis that mainly affects sweat glands.
Linking Hyperhidrosis and Hyperthyroidism
Hyperhidrosis is excessive sweating often linked to autonomic nervous system dysfunction, while hyperthyroidism causes increased metabolic activity that can trigger secondary hyperhidrosis. The overproduction of thyroid hormones in hyperthyroidism stimulates sweat glands, leading to persistent sweating that mimics primary hyperhidrosis symptoms. Understanding the connection between hyperhidrosis and hyperthyroidism helps differentiate primary idiopathic cases from those caused by thyroid hormone imbalances.
Primary vs Secondary Hyperhidrosis Explained
Primary hyperhidrosis is characterized by excessive sweating that occurs without an underlying medical condition, often localized to areas such as the palms, soles, or underarms, and is typically linked to overactive sweat glands. Secondary hyperhidrosis is caused by an underlying condition like hyperthyroidism, which leads to generalized sweating due to increased metabolic activity and hormonal imbalance. Differentiating between primary and secondary hyperhidrosis is crucial for effective treatment, as managing hyperthyroidism can alleviate secondary hyperhidrosis symptoms, whereas primary hyperhidrosis may require targeted therapies such as antiperspirants or botulinum toxin injections.
Clinical Symptoms: Hyperhidrosis Alone vs With Hyperthyroidism
Hyperhidrosis alone manifests as excessive sweating localized primarily to the palms, soles, and underarms without systemic symptoms. In contrast, hyperhidrosis associated with hyperthyroidism presents with generalized sweating alongside other clinical signs such as tachycardia, weight loss, and heat intolerance. Differentiating the sweating pattern and accompanying systemic symptoms is crucial for accurate diagnosis and targeted treatment.
Diagnostic Criteria for Hyperhidrosis and Hyperthyroidism
Hyperhidrosis is diagnosed primarily through clinical evaluation, with criteria including excessive sweating for at least six months without apparent cause, affecting symmetric body areas and interfering with daily activities. Hyperthyroidism diagnosis relies on biochemical tests, such as suppressed thyroid-stimulating hormone (TSH) levels and elevated free thyroxine (FT4) or triiodothyronine (T3). Differentiating hyperhidrosis from hyperthyroidism involves assessing thyroid function tests to exclude thyroid hormone imbalance as the cause of excessive sweating.
Common Causes of Excessive Sweating
Excessive sweating in hyperhidrosis primarily results from overactive sweat glands triggered by genetic factors or nervous system dysfunction, whereas in hyperthyroidism, it stems from an accelerated metabolism due to elevated thyroid hormone levels. Both conditions can cause significant sweating, but hyperthyroidism-related sweating often accompanies symptoms like weight loss, rapid heartbeat, and heat intolerance. Identifying the underlying cause is crucial for targeted treatment, as hyperhidrosis treatments focus on sweat gland activity, while hyperthyroidism requires regulating thyroid function.
Treatment Options: Managing Both Conditions
Treatment options for hyperhidrosis and hyperthyroidism require distinct approaches due to their different underlying causes; managing hyperhidrosis often includes antiperspirants, iontophoresis, or botulinum toxin injections, while hyperthyroidism typically demands antithyroid medications, radioactive iodine therapy, or thyroidectomy. Addressing hyperthyroidism with proper endocrine management can often reduce secondary hyperhidrosis symptoms caused by thyroid hormone excess. Combining targeted therapies ensures effective control of excessive sweating while stabilizing thyroid function.
Prognosis: Hyperhidrosis with Hyperthyroidism Compared
Hyperhidrosis secondary to hyperthyroidism often shows improvement once thyroid hormone levels are normalized, indicating a generally favorable prognosis with appropriate endocrine treatment. In contrast, primary hyperhidrosis typically persists chronically without underlying systemic causes, requiring targeted therapies such as antiperspirants, iontophoresis, or botulinum toxin injections for symptom management. Prognosis varies significantly as hyperhidrosis associated with hyperthyroidism tends to resolve with thyroid control, while primary hyperhidrosis usually demands ongoing symptom-focused interventions.
When to See a Specialist for Excessive Sweating
Excessive sweating can be a symptom of hyperhidrosis, a condition characterized by abnormal sweating, or it may result from hyperthyroidism, where an overactive thyroid gland increases metabolism and perspiration. When sweating is persistent, occurs without obvious triggers, or is accompanied by other symptoms such as unexplained weight loss, rapid heartbeat, or heat intolerance, it is important to see an endocrinologist to evaluate for hyperthyroidism. Consulting a dermatologist is crucial if excessive sweating is localized, severely impacts daily activities, or does not respond to over-the-counter treatments, as specialized management for hyperhidrosis may be required.
Hyperhidrosis and hyperthyroidism Infographic
 libterm.com
libterm.com