Scar formation occurs as the body repairs damaged skin by producing collagen fibers to close wounds, resulting in a visible mark. The appearance and texture of scars vary depending on the injury type, location, and individual healing processes. Explore the rest of the article to understand how different factors influence scar development and effective treatments for minimizing their impact on your skin.
Table of Comparison
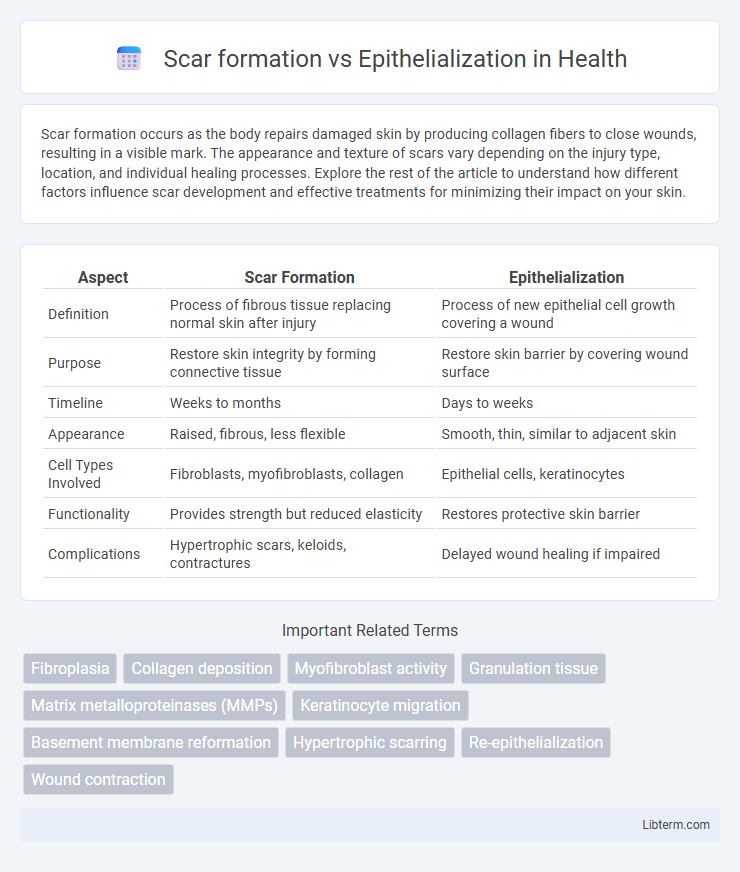
| Aspect | Scar Formation | Epithelialization |
|---|---|---|
| Definition | Process of fibrous tissue replacing normal skin after injury | Process of new epithelial cell growth covering a wound |
| Purpose | Restore skin integrity by forming connective tissue | Restore skin barrier by covering wound surface |
| Timeline | Weeks to months | Days to weeks |
| Appearance | Raised, fibrous, less flexible | Smooth, thin, similar to adjacent skin |
| Cell Types Involved | Fibroblasts, myofibroblasts, collagen | Epithelial cells, keratinocytes |
| Functionality | Provides strength but reduced elasticity | Restores protective skin barrier |
| Complications | Hypertrophic scars, keloids, contractures | Delayed wound healing if impaired |
Introduction to Wound Healing Processes
Wound healing encompasses multiple overlapping phases, with epithelialization restoring the skin's surface by generating new epithelial cells, while scar formation results from the fibroblast-driven deposition of collagen in the dermis. Epithelialization is critical for reestablishing the protective barrier, occurring primarily within days after injury, whereas scar formation reflects the remodeling phase that can last weeks to months. Effective wound repair balances these processes to optimize tissue integrity and function, minimizing fibrotic scar tissue while promoting rapid epithelial coverage.
Defining Scar Formation
Scar formation is the biological process of replacing normal skin tissue with fibrous connective tissue following an injury, leading to a permanent mark known as a scar. This process involves fibroblast activation, collagen deposition, and extracellular matrix remodeling, which restore tissue integrity but often reduce skin elasticity and function. In contrast, epithelialization is the restoration of the skin's surface layer through keratinocyte migration and proliferation, contributing to wound closure without necessarily forming a scar.
Understanding Epithelialization
Epithelialization is the critical process in wound healing where epithelial cells migrate across the wound bed to restore the skin barrier, promoting tissue regeneration without fibrosis. Unlike scar formation, which involves excessive collagen deposition and leads to fibrous, less functional tissue, epithelialization aims for restoration of normal skin architecture and function. Efficient epithelialization depends on factors such as adequate moisture, oxygen supply, and minimal infection to encourage rapid closure and minimize scarring.
Key Biological Mechanisms
Scar formation involves fibroblast proliferation, collagen deposition, and extracellular matrix remodeling, resulting in dense, fibrotic tissue that restores structural integrity but lacks original skin appendages. Epithelialization is characterized by keratinocyte migration, proliferation, and differentiation from wound edges, re-establishing the epidermal barrier and promoting tissue regeneration without fibrosis. Key biological mechanisms include transforming growth factor-beta (TGF-b) signaling driving fibrosis in scar formation, while growth factors like epidermal growth factor (EGF) and vascular endothelial growth factor (VEGF) enhance epithelialization and angiogenesis.
Phases of Wound Healing
Scar formation and epithelialization represent distinct phases of wound healing, with epithelialization primarily occurring during the proliferative phase, where keratinocytes migrate to cover the wound bed and restore the epidermal barrier. Scar formation is a hallmark of the remodeling phase, characterized by collagen deposition and matrix remodeling that restore tissue strength but often result in fibrotic tissue. Effective wound healing depends on the coordinated transition from epithelialization to scar formation, balancing tissue regeneration and structural repair.
Factors Influencing Scar Formation
Scar formation is influenced by factors such as the depth and size of the wound, tension on the skin, and individual genetic predisposition. In contrast, epithelialization depends on the migration and proliferation of keratinocytes from wound edges, which can be affected by moisture levels and the presence of infection. Understanding the balance between collagen deposition in scar tissue and epithelial cell regeneration is critical for optimizing wound healing outcomes.
Factors Impacting Epithelialization
Epithelialization is critically influenced by factors such as adequate oxygen supply, moisture balance, and the presence of essential growth factors like epidermal growth factor (EGF) which promote keratinocyte migration and proliferation. Scar formation occurs when the epithelial layer fails to regenerate properly, often due to prolonged inflammation, infection, or impaired fibroblast function that disrupts the extracellular matrix remodeling. Controlling wound environment, managing infection, and ensuring sufficient nutrition, including vitamins A and C, significantly enhance epithelialization and minimize excessive scar tissue development.
Clinical Differences Between Scarring and Epithelialization
Scar formation involves the deposition of dense collagen fibers leading to fibrous tissue that lacks normal skin appendages, whereas epithelialization is the process of keratinocyte migration restoring the epidermal barrier without substantial fibrosis. Clinically, scars present as raised, discolored, and less elastic areas often accompanied by altered sensation, while epithelialized skin appears smooth, closely resembling the surrounding tissue with normal function and texture. The distinction in healing outcomes impacts treatment decisions, with epithelialization preferred for functional and aesthetic restoration.
Implications for Treatment and Recovery
Scar formation results from fibroblast proliferation and collagen deposition that restore tissue integrity but reduce elasticity, often leading to functional and cosmetic concerns. Epithelialization involves keratinocyte migration over wounds, promoting barrier restoration with minimal scarring, crucial for rapid recovery in superficial injuries. Treatment strategies targeting reduced fibroblast activity and enhanced epithelial cell regeneration improve healing outcomes and minimize scar-related complications.
Recent Advances in Wound Healing Research
Recent advances in wound healing research highlight the dichotomy between scar formation and epithelialization, emphasizing molecular pathways that promote regenerative healing over fibrotic scarring. Studies on growth factors such as TGF-b3 and matrix metalloproteinases have demonstrated their critical roles in reducing collagen deposition and enhancing epithelial cell migration, thus favoring scarless repair. Cutting-edge therapies including stem cell applications and biomaterial scaffolds show promising potential to modulate the wound microenvironment, accelerating epithelialization while minimizing hypertrophic scar development.
Scar formation Infographic
 libterm.com
libterm.com