Inflammation is the body's natural response to injury or infection, characterized by redness, swelling, heat, and pain as immune cells work to protect and heal affected tissues. Chronic inflammation, however, can contribute to various health issues such as heart disease, arthritis, and autoimmune disorders. Explore the rest of the article to understand how managing inflammation can improve your overall well-being.
Table of Comparison
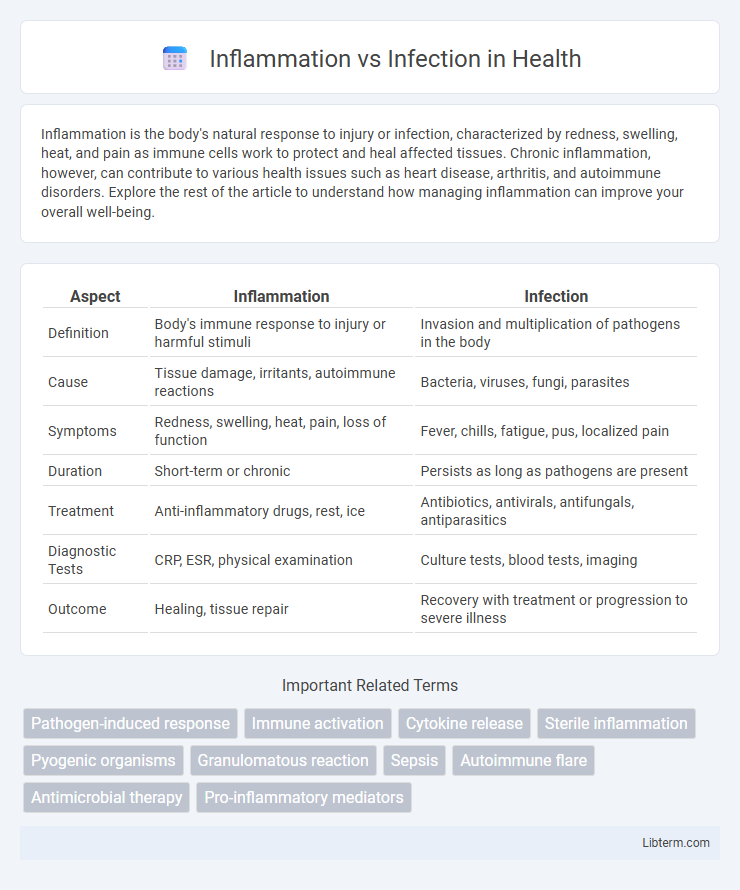
| Aspect | Inflammation | Infection |
|---|---|---|
| Definition | Body's immune response to injury or harmful stimuli | Invasion and multiplication of pathogens in the body |
| Cause | Tissue damage, irritants, autoimmune reactions | Bacteria, viruses, fungi, parasites |
| Symptoms | Redness, swelling, heat, pain, loss of function | Fever, chills, fatigue, pus, localized pain |
| Duration | Short-term or chronic | Persists as long as pathogens are present |
| Treatment | Anti-inflammatory drugs, rest, ice | Antibiotics, antivirals, antifungals, antiparasitics |
| Diagnostic Tests | CRP, ESR, physical examination | Culture tests, blood tests, imaging |
| Outcome | Healing, tissue repair | Recovery with treatment or progression to severe illness |
Understanding Inflammation: Definition and Key Features
Inflammation is the body's complex biological response to harmful stimuli such as pathogens, damaged cells, or irritants, characterized by redness, heat, swelling, and pain. It involves the activation of immune cells, release of signaling molecules like cytokines, and increased blood flow to affected tissues to facilitate healing and defense. Unlike infection, which is caused by the invasion of pathogens, inflammation is a protective mechanism that can occur independently of infection.
What Is Infection? Causes and Mechanisms
Infection is the invasion and multiplication of pathogenic microorganisms such as bacteria, viruses, fungi, or parasites within the body, leading to tissue damage and immune response activation. Causes of infection include exposure to infectious agents through contaminated surfaces, airborne droplets, bodily fluids, or wounds. Mechanisms involve pathogen entry, evasion of the host immune system, and replication, which trigger inflammatory processes aimed at eliminating the infectious agents.
Comparing Inflammation and Infection: Core Differences
Inflammation is the body's immune response to harmful stimuli, characterized by redness, swelling, heat, and pain, while infection involves the invasion and multiplication of pathogens such as bacteria, viruses, or fungi in body tissues. Inflammation can occur without infection, serving as a protective mechanism to initiate healing, whereas infection always involves microbial presence triggering the immune response. Understanding the distinction between sterile inflammation and pathogen-induced infection is crucial for accurate diagnosis and effective treatment strategies.
Common Causes of Inflammation vs Infection
Common causes of inflammation include physical injury, autoimmune reactions, exposure to irritants such as chemicals or allergens, and chronic conditions like arthritis. Infection, on the other hand, is primarily caused by pathogenic microorganisms such as bacteria, viruses, fungi, and parasites invading the body. While inflammation is the body's immune response to various harmful stimuli, infection specifically results from microbial invasion and proliferation.
Symptoms: How Inflammation Differs from Infection
Inflammation manifests with redness, heat, swelling, pain, and loss of function as the body's immune response to injury or irritants, while infection presents with similar symptoms but includes the presence of pathogens like bacteria, viruses, or fungi. Fever, pus formation, and systemic symptoms such as chills or fatigue are more indicative of infection compared to sterile inflammation. Recognizing these differences is crucial for accurate diagnosis and appropriate treatment strategies.
Diagnostic Approaches for Inflammation and Infection
Diagnostic approaches for inflammation include measuring biomarkers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), alongside imaging techniques like ultrasound and MRI to identify tissue swelling and damage. Infection diagnosis relies on microbiological cultures, polymerase chain reaction (PCR) assays, and serological tests to detect specific pathogens, coupled with clinical examination and symptom assessment. Combining laboratory findings with patient history enhances differentiation between inflammation caused by sterile injury and infection-driven immune responses.
Treatment Strategies: Inflammation vs Infection
Treatment strategies for inflammation primarily involve anti-inflammatory medications such as NSAIDs, corticosteroids, and lifestyle modifications targeting the underlying cause. Infection treatment requires targeted antimicrobial therapies, including antibiotics, antivirals, or antifungals, depending on the pathogen involved. Accurate diagnosis distinguishing inflammation from infection is crucial to avoid inappropriate use of antimicrobials and ensure effective management.
Preventive Measures for Both Conditions
Preventive measures for inflammation and infection emphasize maintaining a healthy lifestyle with balanced nutrition, regular exercise, and adequate hydration to support immune function and reduce the risk of chronic inflammation. Proper hygiene practices, including regular handwashing and wound care, help prevent infection by minimizing exposure to pathogens. Vaccinations, stress management, and avoiding smoking further contribute to reducing susceptibility to both inflammatory responses and infectious diseases.
Complications and Risks Linked to Inflammation and Infection
Inflammation can lead to chronic conditions such as arthritis, cardiovascular disease, and tissue damage if uncontrolled, while infections risk spreading pathogens that cause sepsis or systemic inflammatory response syndrome. Persistent inflammation may cause fibrosis and organ dysfunction, whereas infections can trigger antibiotic resistance and multiple organ failure. Both conditions heighten the risk of impaired immune function, complicating recovery and increasing morbidity and mortality rates.
When to Seek Medical Advice: Red Flags and Warning Signs
Persistent fever above 101.3degF (38.5degC), swelling with severe pain, or red streaks spreading from the affected area signal potential infection requiring immediate medical attention. Inflammation accompanied by difficulty breathing, chest pain, confusion, or sudden weakness may indicate serious systemic involvement and warrants urgent evaluation. Seek prompt medical advice if symptoms worsen rapidly or do not improve within 48 hours despite home care.
Inflammation Infographic
 libterm.com
libterm.com