Hemothorax is a condition where blood accumulates in the pleural cavity, often resulting from trauma or injury to the chest. Prompt diagnosis and treatment are crucial to prevent respiratory distress and complications such as infection or fibrosis. Explore the rest of the article to understand the causes, symptoms, and effective management of hemothorax to protect your health.
Table of Comparison
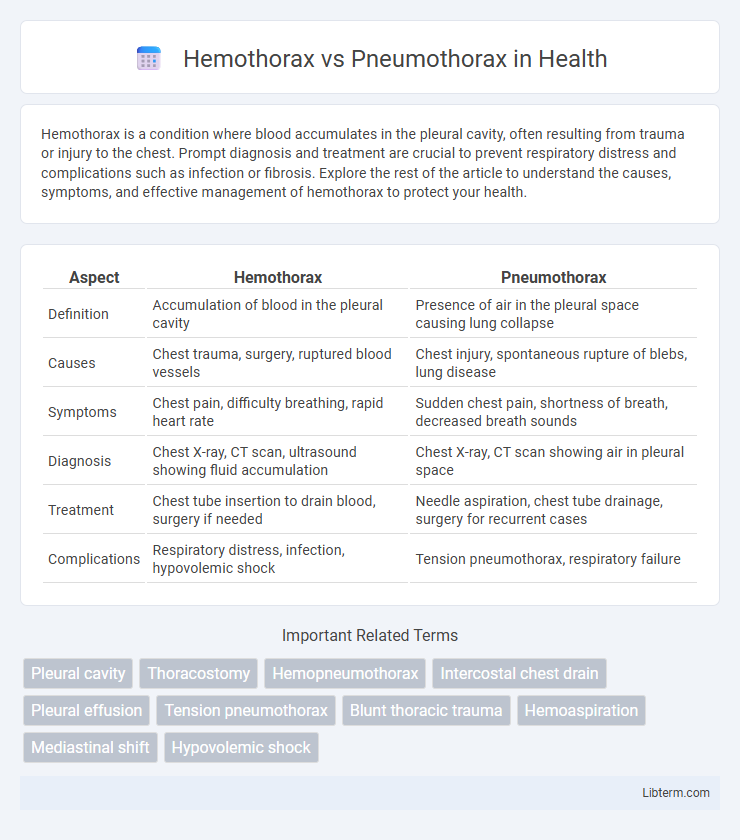
| Aspect | Hemothorax | Pneumothorax |
|---|---|---|
| Definition | Accumulation of blood in the pleural cavity | Presence of air in the pleural space causing lung collapse |
| Causes | Chest trauma, surgery, ruptured blood vessels | Chest injury, spontaneous rupture of blebs, lung disease |
| Symptoms | Chest pain, difficulty breathing, rapid heart rate | Sudden chest pain, shortness of breath, decreased breath sounds |
| Diagnosis | Chest X-ray, CT scan, ultrasound showing fluid accumulation | Chest X-ray, CT scan showing air in pleural space |
| Treatment | Chest tube insertion to drain blood, surgery if needed | Needle aspiration, chest tube drainage, surgery for recurrent cases |
| Complications | Respiratory distress, infection, hypovolemic shock | Tension pneumothorax, respiratory failure |
Introduction to Hemothorax and Pneumothorax
Hemothorax involves the accumulation of blood in the pleural cavity, often caused by trauma or injury to the chest, leading to impaired lung expansion and respiratory distress. Pneumothorax is characterized by the presence of air in the pleural space, resulting in partial or complete lung collapse, commonly due to blunt or penetrating chest trauma, or spontaneous rupture of blebs. Both conditions require prompt diagnosis through imaging such as chest X-ray or CT scan and urgent intervention to restore normal lung function and prevent complications.
Definition and Key Differences
Hemothorax is the accumulation of blood in the pleural cavity, often caused by trauma or chest injury, whereas pneumothorax involves the presence of air in the pleural space, leading to lung collapse. Key differences include the type of fluid--blood in hemothorax and air in pneumothorax--and the clinical presentation, with hemothorax typically presenting with signs of blood loss and pneumothorax causing respiratory distress due to lung compression. Diagnostic imaging such as chest X-ray or CT scan differentiates them by revealing fluid levels in hemothorax and air pockets in pneumothorax.
Causes and Risk Factors
Hemothorax typically results from traumatic injury to the chest, such as rib fractures or penetrating wounds, leading to blood accumulation in the pleural cavity. Pneumothorax often arises due to spontaneous rupture of alveoli or lung blebs, especially in tall, thin individuals or those with underlying lung diseases like chronic obstructive pulmonary disease (COPD). Both conditions share risk factors including chest trauma, invasive procedures, and mechanical ventilation, but their pathophysiology differs with hemothorax involving blood and pneumothorax involving air in the pleural space.
Pathophysiology Overview
Hemothorax involves the accumulation of blood in the pleural cavity, often due to trauma or injury to thoracic blood vessels, leading to impaired lung expansion and hypoxemia. Pneumothorax is characterized by the presence of air within the pleural space, resulting from a breach in the visceral or parietal pleura, causing lung collapse and compromised ventilation. Both conditions disrupt normal pleural pressure dynamics, impair gas exchange, and cause respiratory distress, but hemothorax features blood accumulation while pneumothorax involves air intrusion.
Clinical Presentation and Symptoms
Hemothorax typically presents with chest pain, dyspnea, and signs of hypovolemic shock due to blood accumulation in the pleural space, while pneumothorax often manifests as sudden unilateral chest pain and respiratory distress caused by air in the pleural cavity. Clinical examination in hemothorax reveals diminished breath sounds and dullness to percussion, contrasting with the hyperresonance and decreased breath sounds noted in pneumothorax. Vital signs may show tachycardia and hypotension in hemothorax, whereas pneumothorax symptoms vary based on severity, ranging from mild tachypnea to severe respiratory compromise.
Diagnostic Approaches
Hemothorax diagnosis primarily involves chest X-rays revealing fluid levels, with ultrasound and CT scans offering detailed visualization of blood accumulation in the pleural cavity. Pneumothorax diagnosis relies on chest radiography to identify air presence outside the lung and ultrasound for rapid bedside assessment, particularly in trauma settings. Advanced imaging such as CT scans provides precise evaluation of lung collapse extent and underlying causes for both conditions.
Radiologic and Imaging Findings
Hemothorax appears on chest X-rays as a homogenous opacity with a meniscus sign often layering in the pleural space, indicating fluid accumulation, while computed tomography (CT) scans more precisely delineate the collection of blood with attenuation values typically between 30-45 Hounsfield units. Pneumothorax is characterized by the presence of visceral pleural line with absence of lung markings peripheral to this line on radiographs, and CT imaging confirms air in the pleural space with clear lung retraction and possible identification of small pneumothoraces not visible on X-ray. Ultrasound can detect hemothorax by visualizing anechoic or hypoechoic pleural fluid and pneumothorax through the absence of lung sliding and presence of the "barcode" or "stratosphere" sign on M-mode imaging.
Treatment and Management Strategies
Hemothorax treatment primarily involves chest tube insertion to drain blood and prevent lung compression, with surgical intervention needed for ongoing bleeding or clotted hemothorax. Pneumothorax management varies from observation in small, stable cases to needle aspiration or chest tube placement for larger or symptomatic pneumothorax, with surgery considered for recurrent or persistent air leaks. Both conditions require close monitoring of respiratory status and oxygen supplementation to optimize lung re-expansion and prevent complications.
Prognosis and Potential Complications
Hemothorax prognosis depends on the volume of blood accumulation and timely drainage, with complications including infection, fibrothorax, and respiratory failure. Pneumothorax prognosis varies by size and cause, with potential complications such as tension pneumothorax, recurrent lung collapse, and hypoxemia. Early intervention improves outcomes for both conditions, while delayed treatment increases risk of chronic lung damage and compromised respiratory function.
Prevention and Patient Education
Preventing hemothorax involves minimizing trauma risks through safety measures such as wearing seat belts, protective gear, and avoiding high-risk activities. Patient education emphasizes recognizing symptoms like chest pain and shortness of breath promptly, seeking immediate medical care to reduce complications. Pneumothorax prevention focuses on avoiding smoking, managing lung diseases, and educating patients on early signs such as sudden chest pain and breathlessness for timely intervention.
Hemothorax Infographic
 libterm.com
libterm.com