Oral submucous fibrosis is a chronic, progressive condition characterized by the stiffening of the oral mucosa due to fibrous tissue formation, leading to restricted mouth opening and difficulty in eating or speaking. This disease is primarily linked to areca nut chewing and poses a risk of malignant transformation if left untreated. Discover more about the causes, symptoms, and treatment options to protect your oral health in the rest of this article.
Table of Comparison
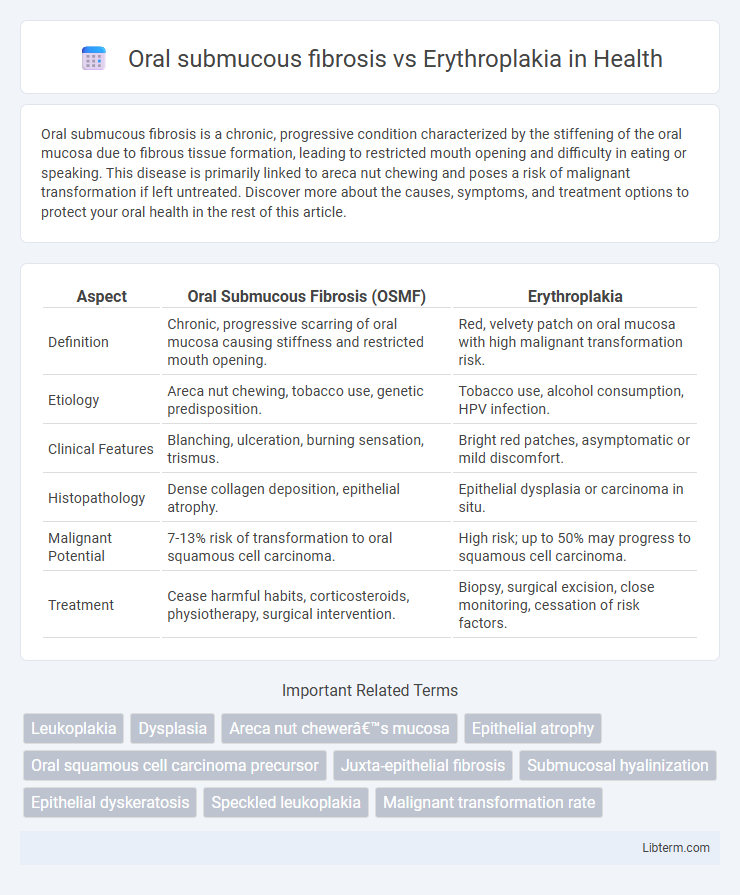
| Aspect | Oral Submucous Fibrosis (OSMF) | Erythroplakia |
|---|---|---|
| Definition | Chronic, progressive scarring of oral mucosa causing stiffness and restricted mouth opening. | Red, velvety patch on oral mucosa with high malignant transformation risk. |
| Etiology | Areca nut chewing, tobacco use, genetic predisposition. | Tobacco use, alcohol consumption, HPV infection. |
| Clinical Features | Blanching, ulceration, burning sensation, trismus. | Bright red patches, asymptomatic or mild discomfort. |
| Histopathology | Dense collagen deposition, epithelial atrophy. | Epithelial dysplasia or carcinoma in situ. |
| Malignant Potential | 7-13% risk of transformation to oral squamous cell carcinoma. | High risk; up to 50% may progress to squamous cell carcinoma. |
| Treatment | Cease harmful habits, corticosteroids, physiotherapy, surgical intervention. | Biopsy, surgical excision, close monitoring, cessation of risk factors. |
Introduction to Oral Submucous Fibrosis and Erythroplakia
Oral submucous fibrosis (OSF) is a chronic, progressive scarring condition of the oral mucosa associated with areca nut chewing, characterized by reduced mouth opening and a high malignant transformation rate. Erythroplakia presents as a red, velvety patch in the oral cavity with a significant risk of severe epithelial dysplasia or carcinoma in situ, often linked to tobacco use. Both conditions require early diagnosis and intervention due to their potential for malignant transformation in the oral epithelium.
Epidemiology and Prevalence
Oral submucous fibrosis (OSMF) predominantly affects populations in South Asia, with prevalence rates ranging from 0.2% to 0.5% in India, largely attributed to areca nut chewing habits. Erythroplakia, although less common, has a prevalence of approximately 0.02% to 0.83% globally, with higher incidences reported in smokers and heavy alcohol users. Both conditions exhibit a higher occurrence in males aged 30-50 years, with OSMF demonstrating a progressively increasing trend due to lifestyle factors.
Etiology and Risk Factors
Oral submucous fibrosis primarily results from areca nut chewing, commonly combined with tobacco use, leading to chronic inflammation and progressive fibrosis in the oral mucosa. Erythroplakia, a distinct premalignant lesion, is strongly associated with tobacco smoking, alcohol consumption, and HPV infection, causing localized epithelial dysplasia. Both conditions share risk factors like tobacco but differ etiologically, with oral submucous fibrosis linked to betel quid components and erythroplakia to carcinogenic exposures triggering epithelial atrophy and neoplastic transformation.
Clinical Features and Presentation
Oral submucous fibrosis presents with progressive trismus, blanching, and stiffening of the oral mucosa, alongside burning sensation exacerbated by spicy food, commonly affecting the buccal mucosa and soft palate. Erythroplakia is characterized by a well-demarcated, velvety red patch with a high risk of dysplasia or carcinoma, typically occurring on the floor of the mouth, ventral tongue, or soft palate. Both conditions require thorough clinical evaluation due to their potential for malignant transformation but differ significantly in mucosal texture, color, and trismus presence.
Pathogenesis and Molecular Mechanisms
Oral submucous fibrosis (OSF) involves chronic inflammation and excessive collagen deposition triggered by areca nut alkaloids, leading to fibrosis through the activation of fibroblasts and upregulation of transforming growth factor-beta (TGF-b). Erythroplakia represents a dysplastic mucosal lesion with alterations in cell cycle regulators such as p53 mutations and increased expression of matrix metalloproteinases (MMPs), promoting epithelial atrophy and neoplastic transformation. Both conditions share oxidative stress and inflammatory cytokine involvement but differ in that OSF predominantly shows fibrotic pathogenesis while erythroplakia focuses on epithelial dysplasia and malignant potential.
Histopathological Differences
Oral submucous fibrosis exhibits dense collagen deposition with juxta-epithelial inflammatory infiltrates and epithelial atrophy or hyperplasia, often showing early signs of epithelial dysplasia. Erythroplakia histopathology is characterized by a predominantly dysplastic or carcinomatous epithelium with red, erythematous mucosa due to increased vascularity and thinning of the epithelium. While oral submucous fibrosis primarily involves fibrotic submucosal changes, erythroplakia is notable for marked epithelial atypia without significant fibrous tissue alteration.
Malignant Transformation Potential
Oral submucous fibrosis exhibits a high malignant transformation rate, estimated between 7% and 13%, primarily due to chronic inflammation and fibrosis affecting the oral mucosa. Erythroplakia carries a significantly higher risk, with malignant transformation rates reported up to 90%, often representing severe epithelial dysplasia or carcinoma in situ. Early detection and biopsy are critical in both conditions to prevent progression to oral squamous cell carcinoma.
Diagnostic Approaches
Oral submucous fibrosis diagnosis relies on clinical evaluation of mucosal rigidity, blanching, and restricted mouth opening, complemented by biopsy showing epithelial atrophy and juxtaepithelial fibrosis. Erythroplakia diagnosis emphasizes visual identification of well-demarcated red patches, followed by histopathological examination revealing dysplasia or carcinoma in situ. Adjunctive diagnostic tools such as toluidine blue staining, autofluorescence imaging, and cytology enhance early detection and differentiation between these potentially malignant disorders.
Treatment Modalities
Oral submucous fibrosis treatment involves cessation of areca nut chewing, administration of corticosteroids, hyaluronidase injections, and surgical intervention in advanced stages to improve mouth opening. Erythroplakia management requires prompt biopsy due to its high malignant potential, followed by surgical excision, often supplemented with laser therapy or radiotherapy depending on dysplasia severity. Both conditions necessitate regular follow-up to monitor for malignant transformation and ensure effective disease control.
Prognosis and Follow-up Strategies
Oral submucous fibrosis (OSMF) has a progressive nature with a malignant transformation rate of approximately 7-13%, necessitating regular clinical and histopathological monitoring to detect early signs of dysplasia or carcinoma. Erythroplakia exhibits a higher risk of malignancy, with transformation rates up to 50%, requiring more rigorous follow-up, including biopsy and serial evaluations every 3 to 6 months for suspicious lesions. Long-term follow-up strategies for both conditions emphasize early detection, patient education on risk factor cessation, and multidisciplinary management to improve prognosis and reduce progression to oral squamous cell carcinoma.
Oral submucous fibrosis Infographic
 libterm.com
libterm.com