Chronic Venous Insufficiency (CVI) occurs when your leg veins struggle to return blood to the heart, causing swelling, pain, and skin changes. Treatments range from lifestyle adjustments like exercise and compression stockings to medical procedures that improve circulation. Discover effective strategies to manage CVI and improve your quality of life by reading the full article.
Table of Comparison
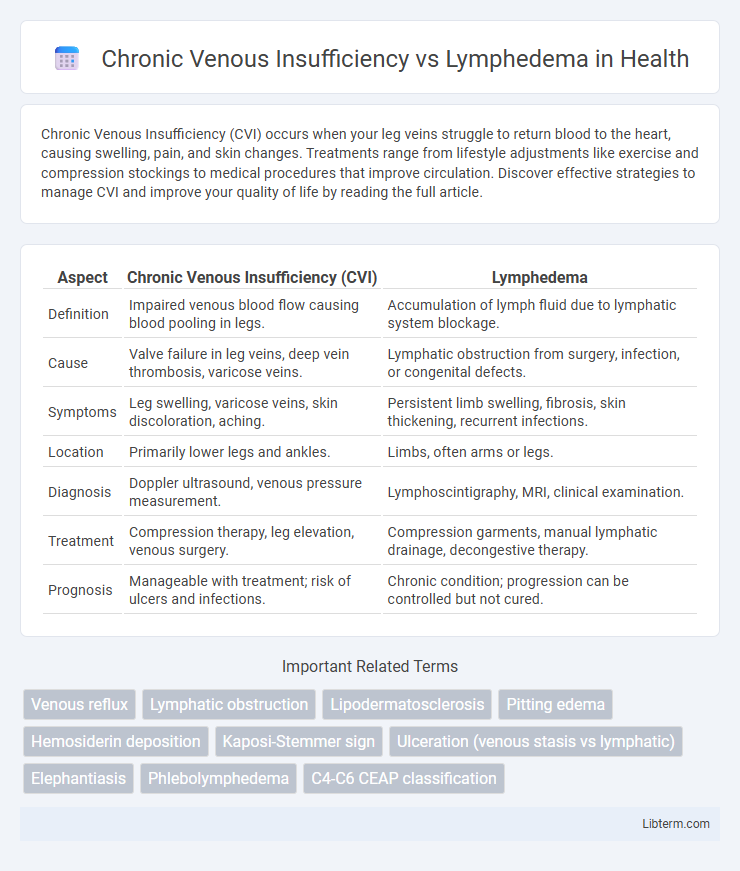
| Aspect | Chronic Venous Insufficiency (CVI) | Lymphedema |
|---|---|---|
| Definition | Impaired venous blood flow causing blood pooling in legs. | Accumulation of lymph fluid due to lymphatic system blockage. |
| Cause | Valve failure in leg veins, deep vein thrombosis, varicose veins. | Lymphatic obstruction from surgery, infection, or congenital defects. |
| Symptoms | Leg swelling, varicose veins, skin discoloration, aching. | Persistent limb swelling, fibrosis, skin thickening, recurrent infections. |
| Location | Primarily lower legs and ankles. | Limbs, often arms or legs. |
| Diagnosis | Doppler ultrasound, venous pressure measurement. | Lymphoscintigraphy, MRI, clinical examination. |
| Treatment | Compression therapy, leg elevation, venous surgery. | Compression garments, manual lymphatic drainage, decongestive therapy. |
| Prognosis | Manageable with treatment; risk of ulcers and infections. | Chronic condition; progression can be controlled but not cured. |
Introduction to Chronic Venous Insufficiency and Lymphedema
Chronic Venous Insufficiency (CVI) is a condition where damaged valves in the leg veins cause blood to pool, leading to symptoms such as swelling, pain, and skin changes. Lymphedema results from impaired lymphatic drainage, causing persistent limb swelling due to the accumulation of lymph fluid. Both disorders manifest as lower extremity swelling but differ in pathophysiology, with CVI primarily involving venous valve failure and lymphedema involving lymphatic system dysfunction.
Understanding the Underlying Causes
Chronic Venous Insufficiency (CVI) primarily results from malfunctioning valves in the veins, leading to blood pooling and increased venous pressure in the lower extremities. Lymphedema occurs due to impaired lymphatic drainage, often caused by lymph node removal, infection, or congenital abnormalities, resulting in fluid accumulation and swelling. Differentiating these conditions hinges on understanding that CVI involves venous system failure while lymphedema stems from lymphatic system dysfunction.
Key Differences in Pathophysiology
Chronic Venous Insufficiency (CVI) results from incompetent venous valves causing blood pooling and increased venous pressure, leading to edema and skin changes primarily in the lower extremities. In contrast, lymphedema arises from impaired lymphatic drainage due to lymphatic vessel damage or obstruction, causing protein-rich fluid accumulation and tissue swelling. CVI involves venous hypertension and valve dysfunction, whereas lymphedema is characterized by lymphatic system failure and often presents with a non-pitting edema distinct from the venous swelling seen in CVI.
Typical Signs and Symptoms
Chronic Venous Insufficiency (CVI) typically presents with symptoms such as leg swelling, aching, skin discoloration, and varicose veins, often worsening after prolonged standing. Lymphedema is characterized by persistent, non-pitting swelling, usually in the limbs, accompanied by a heavy or tight sensation and skin thickening or fibrosis in advanced stages. While CVI primarily affects venous return causing pigmentation changes and ulcers, lymphedema involves lymphatic system dysfunction leading to fluid accumulation and a distinct "woody" skin texture.
Diagnostic Approaches and Tools
Chronic Venous Insufficiency (CVI) diagnosis primarily relies on duplex ultrasonography to assess venous reflux and valve dysfunction, while Lymphedema diagnosis uses lymphoscintigraphy to visualize lymphatic flow and identify obstructions. Physical examination combined with patient history is essential for both, but CVI often presents with varicose veins and skin changes, whereas Lymphedema shows persistent limb swelling without significant venous abnormalities. Advanced imaging modalities like MRI and CT scans can further differentiate between the two by highlighting vascular versus lymphatic system impairments.
Risk Factors and Predisposing Conditions
Chronic Venous Insufficiency (CVI) primarily arises from damaged venous valves, with risk factors including prolonged standing, obesity, deep vein thrombosis, and age-related vein degeneration. Lymphedema results from lymphatic system obstruction or damage, often caused by cancer treatments, infections like filariasis, or surgical lymph node removal. Both conditions share obesity as a common predisposing factor but differ, with CVI linked to venous hypertension and lymphedema associated with impaired lymphatic drainage.
Treatment Modalities for Both Conditions
Chronic venous insufficiency treatment involves compression therapy, leg elevation, and venotonics to improve venous return and reduce symptoms, with sclerotherapy or vein surgery reserved for severe cases. Lymphedema management emphasizes complete decongestive therapy (CDT), including manual lymphatic drainage, compression bandaging, skin care, and specialized exercises to enhance lymphatic flow. Both conditions benefit from tailored physical therapies, but lymphedema requires more intensive drainage techniques and lifelong maintenance to prevent progression.
Complications and Long-term Outcomes
Chronic Venous Insufficiency (CVI) primarily leads to complications such as venous ulcers, skin changes including hyperpigmentation and lipodermatosclerosis, and a heightened risk of deep vein thrombosis, significantly impacting mobility and quality of life. Lymphedema, characterized by lymphatic fluid accumulation, frequently results in recurring infections like cellulitis, permanent tissue fibrosis, and impaired immune function, which can cause progressive limb swelling and functional disability. Long-term outcomes differ as CVI-related ulcers often persist or recur without effective venous intervention, whereas advanced lymphedema can cause irreversible tissue damage and a predisposition to lymphangiosarcoma, underscoring the critical need for early diagnosis and tailored management.
Lifestyle Modifications and Preventive Strategies
Chronic venous insufficiency (CVI) management emphasizes regular leg elevation, compression stockings, and weight management to improve venous return and reduce swelling. Lymphedema requires meticulous skin care, manual lymphatic drainage, and avoidance of limb constriction to prevent infection and fluid buildup. Both conditions benefit from consistent exercise and avoiding prolonged standing or sitting to enhance circulation and lymphatic flow.
Choosing the Right Management Plan
Chronic venous insufficiency (CVI) and lymphedema both require targeted management plans based on their distinct pathophysiologies, with CVI focusing on improving venous return through compression therapy, exercise, and elevation while lymphedema treatment emphasizes lymphatic drainage and meticulous skin care to prevent infections. Accurate diagnosis using duplex ultrasound for CVI and lymphoscintigraphy for lymphedema guides the choice of interventions such as graduated compression stockings for CVI or complete decongestive therapy for lymphedema. Tailoring treatment to the specific condition optimizes symptom control, reduces complications, and improves patient quality of life.
Chronic Venous Insufficiency Infographic
 libterm.com
libterm.com