Hyperkalemia occurs when potassium levels in your blood become elevated beyond normal limits, potentially disrupting heart and muscle function. Causes range from kidney dysfunction and certain medications to excessive potassium intake, making accurate diagnosis and management essential. Explore the rest of this article to understand symptoms, treatment options, and prevention strategies for hyperkalemia.
Table of Comparison
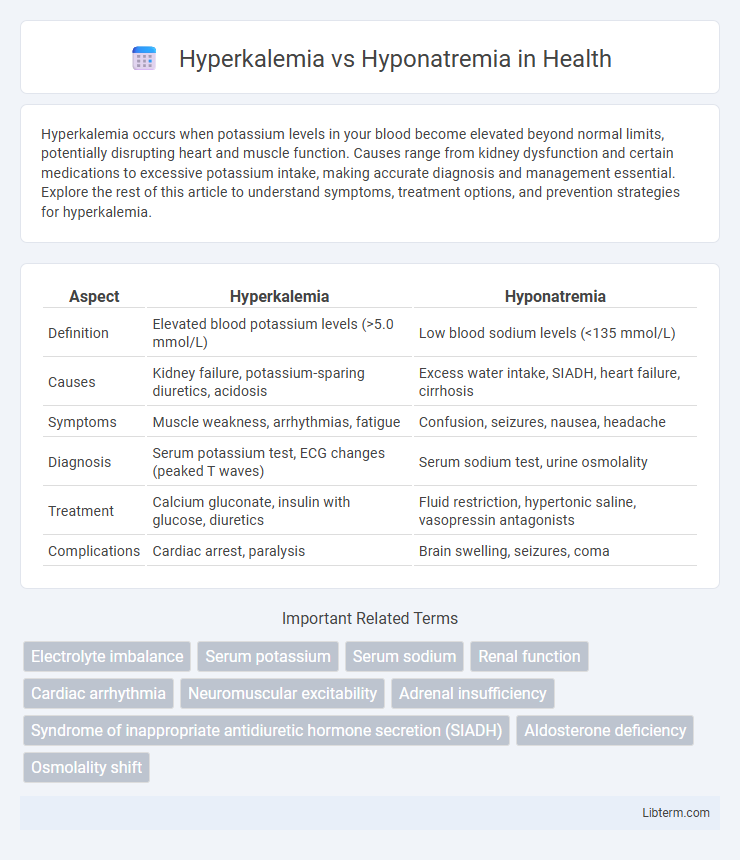
| Aspect | Hyperkalemia | Hyponatremia |
|---|---|---|
| Definition | Elevated blood potassium levels (>5.0 mmol/L) | Low blood sodium levels (<135 mmol/L) |
| Causes | Kidney failure, potassium-sparing diuretics, acidosis | Excess water intake, SIADH, heart failure, cirrhosis |
| Symptoms | Muscle weakness, arrhythmias, fatigue | Confusion, seizures, nausea, headache |
| Diagnosis | Serum potassium test, ECG changes (peaked T waves) | Serum sodium test, urine osmolality |
| Treatment | Calcium gluconate, insulin with glucose, diuretics | Fluid restriction, hypertonic saline, vasopressin antagonists |
| Complications | Cardiac arrest, paralysis | Brain swelling, seizures, coma |
Introduction to Electrolyte Imbalances
Electrolyte imbalances such as hyperkalemia and hyponatremia critically affect cellular function and overall homeostasis, with hyperkalemia characterized by elevated potassium levels above 5.0 mmol/L and hyponatremia defined by sodium levels below 135 mmol/L. These disturbances disrupt myocardial conduction and neuromuscular activity, potentially leading to life-threatening cardiac arrhythmias or neurological deficits. Understanding the pathophysiological mechanisms and clinical presentations of hyperkalemia and hyponatremia is essential for timely diagnosis and effective management.
Understanding Hyperkalemia: Definition and Causes
Hyperkalemia is defined by elevated potassium levels in the blood, typically above 5.0 mmol/L, which can disrupt normal cellular function and cardiac rhythm. Primary causes include kidney failure, potassium-sparing diuretics, adrenal insufficiency, and metabolic acidosis. Unlike hyponatremia, which involves low sodium levels, hyperkalemia directly affects cardiac electrical activity, posing a significant risk for arrhythmias.
Understanding Hyponatremia: Definition and Causes
Hyponatremia is a medical condition characterized by low sodium levels in the blood, typically below 135 mmol/L, which disrupts cellular function and fluid balance. Common causes include excessive fluid intake, congestive heart failure, kidney disease, and syndrome of inappropriate antidiuretic hormone secretion (SIADH), all leading to dilution or loss of sodium. Accurate diagnosis requires blood plasma sodium measurement and assessment of underlying conditions affecting sodium regulation.
Pathophysiological Differences: Potassium vs. Sodium
Hyperkalemia involves elevated potassium levels, disrupting the resting membrane potential and causing impaired neuromuscular function and cardiac conduction abnormalities. In contrast, hyponatremia is characterized by reduced sodium levels, leading to cellular swelling due to osmotic imbalance, particularly affecting the central nervous system. Potassium mainly influences intracellular electrical activity, while sodium governs extracellular fluid volume and osmotic pressure.
Signs and Symptoms of Hyperkalemia
Hyperkalemia manifests with muscle weakness, fatigue, and cardiac arrhythmias, including palpitations and life-threatening ventricular fibrillation. Electrocardiogram changes such as peaked T waves, widened QRS complexes, and prolonged PR intervals are hallmarks distinguishing hyperkalemia. Nausea and numbness or tingling sensations may also occur, contrasting with hyponatremia's predominant neurological symptoms like headache, confusion, and seizures.
Signs and Symptoms of Hyponatremia
Hyponatremia manifests with symptoms including nausea, headache, confusion, and seizures due to low sodium levels disrupting cellular function and causing cerebral edema. Patients often experience fatigue, muscle weakness, and irritability as electrolyte imbalances affect neuromuscular activity. Severe cases may progress to coma or respiratory arrest, highlighting the critical need for prompt diagnosis and management.
Diagnostic Approaches for Hyperkalemia and Hyponatremia
Diagnostic approaches for hyperkalemia primarily involve serum potassium measurement, electrocardiogram (ECG) to detect characteristic changes such as peaked T waves, and assessment of renal function to identify underlying causes like acute kidney injury. Hyponatremia diagnosis requires serum sodium evaluation below 135 mEq/L, measurement of serum and urine osmolality, and clinical assessment of volume status to differentiate between hypovolemic, euvolemic, and hypervolemic states. Both conditions necessitate careful history taking and laboratory tests to guide appropriate management and identify potential life-threatening etiologies.
Treatment Strategies: Hyperkalemia vs. Hyponatremia
Treatment strategies for hyperkalemia prioritize rapid reduction of serum potassium levels through calcium gluconate administration to stabilize cardiac membranes, insulin with glucose to shift potassium intracellularly, and use of potassium-binding agents like sodium polystyrene sulfonate or patiromer. In contrast, hyponatremia management depends on severity and etiology, often involving fluid restriction for euvolemic or hypervolemic states, hypertonic saline infusion in symptomatic or severe cases, and vasopressin receptor antagonists for syndrome of inappropriate antidiuretic hormone secretion (SIADH). Continuous monitoring of electrolyte levels and underlying cause correction are essential in both conditions to prevent complications and achieve electrolyte balance restoration.
Complications and Prognosis
Hyperkalemia can lead to life-threatening cardiac arrhythmias and muscle paralysis, increasing the risk of sudden cardiac death if untreated. Hyponatremia frequently causes neurological complications such as seizures, cerebral edema, and coma, with severity depending on the speed of sodium decline. Both conditions require prompt management to prevent irreversible damage and improve patient prognosis, as delayed treatment significantly worsens outcomes.
Prevention and Patient Education
Prevention of hyperkalemia focuses on managing dietary potassium intake, monitoring kidney function, and adjusting medications that affect potassium levels, such as ACE inhibitors or potassium-sparing diuretics. Preventing hyponatremia involves careful fluid management, avoiding excessive water intake, and close monitoring of sodium levels in patients with heart failure, liver cirrhosis, or SIADH. Patient education emphasizes recognizing symptoms like muscle weakness for hyperkalemia and confusion or seizures for hyponatremia, while encouraging adherence to dietary guidelines and medication regimens to maintain electrolyte balance.
Hyperkalemia Infographic
 libterm.com
libterm.com