Hyperkalemia is a medical condition characterized by elevated potassium levels in the blood, which can disrupt heart function and lead to serious health complications. Prompt diagnosis and management are essential to prevent potentially life-threatening cardiac arrhythmias and muscle weakness. Discover effective treatment options and lifestyle adjustments to protect your health in the rest of this article.
Table of Comparison
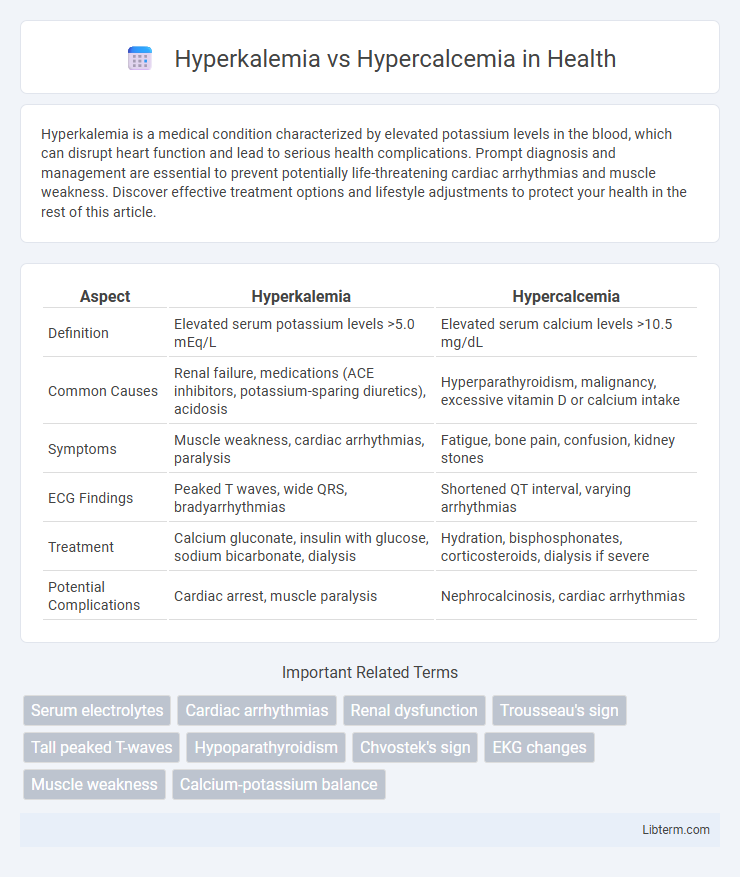
| Aspect | Hyperkalemia | Hypercalcemia |
|---|---|---|
| Definition | Elevated serum potassium levels >5.0 mEq/L | Elevated serum calcium levels >10.5 mg/dL |
| Common Causes | Renal failure, medications (ACE inhibitors, potassium-sparing diuretics), acidosis | Hyperparathyroidism, malignancy, excessive vitamin D or calcium intake |
| Symptoms | Muscle weakness, cardiac arrhythmias, paralysis | Fatigue, bone pain, confusion, kidney stones |
| ECG Findings | Peaked T waves, wide QRS, bradyarrhythmias | Shortened QT interval, varying arrhythmias |
| Treatment | Calcium gluconate, insulin with glucose, sodium bicarbonate, dialysis | Hydration, bisphosphonates, corticosteroids, dialysis if severe |
| Potential Complications | Cardiac arrest, muscle paralysis | Nephrocalcinosis, cardiac arrhythmias |
Introduction to Hyperkalemia and Hypercalcemia
Hyperkalemia is characterized by elevated potassium levels in the bloodstream, typically above 5.0 mmol/L, which can disrupt cardiac and neuromuscular function. Hypercalcemia involves increased calcium concentration, often exceeding 10.5 mg/dL, and is commonly associated with hyperparathyroidism or malignancy. Both electrolyte imbalances require prompt diagnosis to prevent complications such as cardiac arrhythmias and neuromuscular symptoms.
Key Differences: Hyperkalemia vs Hypercalcemia
Hyperkalemia involves elevated potassium levels in the blood, typically above 5.0 mmol/L, often causing muscle weakness, cardiac arrhythmias, and potential cardiac arrest. Hypercalcemia, characterized by high calcium levels above 10.5 mg/dL, leads to symptoms such as kidney stones, bone pain, and neurological disturbances. The primary difference lies in their electrolyte imbalance and clinical manifestations, with hyperkalemia affecting cardiac conduction more acutely and hypercalcemia impacting skeletal and renal systems.
Causes and Risk Factors of Hyperkalemia
Hyperkalemia, characterized by elevated potassium levels in the blood, primarily results from kidney dysfunction, such as chronic kidney disease or acute kidney injury, which impairs potassium excretion. Other causes include the use of potassium-sparing diuretics, excessive potassium intake, adrenal insufficiency (Addison's disease), and cellular breakdown from conditions like rhabdomyolysis or hemolysis. Risk factors for hyperkalemia involve diabetes mellitus, use of ACE inhibitors or ARBs, and severe tissue damage, distinguishing it from hypercalcemia, which is often linked to hyperparathyroidism or malignancies.
Causes and Risk Factors of Hypercalcemia
Hypercalcemia primarily results from hyperparathyroidism, malignancies such as lung or breast cancer, and excessive vitamin D intake. Risk factors include chronic kidney disease, certain medications like thiazide diuretics, and prolonged immobilization. Other causes encompass granulomatous diseases, including sarcoidosis, and endocrine disorders such as hyperthyroidism.
Clinical Manifestations: Comparing Symptoms
Hyperkalemia presents with muscle weakness, fatigue, and cardiac arrhythmias including peaked T waves and widened QRS complexes on ECG. Hypercalcemia typically causes polyuria, kidney stones, bone pain, and neuropsychiatric symptoms such as confusion or depression. Both conditions can induce cardiac abnormalities, but hyperkalemia largely affects conduction velocity, while hypercalcemia influences cardiac contractility and excitability.
Diagnostic Approaches for Both Conditions
Diagnostic approaches for hyperkalemia include serum potassium measurement, electrocardiogram (ECG) analysis showing peaked T waves or widened QRS complexes, and assessment of kidney function to identify underlying causes. Hypercalcemia diagnosis relies on total and ionized serum calcium levels, parathyroid hormone (PTH) testing to distinguish primary hyperparathyroidism, and imaging studies such as bone scans or neck ultrasound for related pathologies. Both conditions require comprehensive laboratory evaluation and clinical correlation for accurate diagnosis and effective management.
Electrocardiogram (ECG) Changes: Hyperkalemia vs Hypercalcemia
Hyperkalemia causes peaked T waves, widened QRS complexes, and flattened P waves on an ECG, often progressing to sine wave patterns and ventricular fibrillation if untreated. Hypercalcemia typically shortens the QT interval by decreasing the ST segment duration, with no significant changes in T wave morphology or QRS width. Recognizing these distinct ECG changes is crucial for timely diagnosis and management of electrolyte imbalances.
Standard Treatment Strategies
Standard treatment strategies for hyperkalemia prioritize rapid stabilization of cardiac membranes using intravenous calcium gluconate, followed by measures to shift potassium intracellularly with insulin and glucose or beta-2 agonists, and enhance potassium elimination through diuretics, sodium polystyrene sulfonate, or dialysis in severe cases. In contrast, hypercalcemia management centers on volume expansion with isotonic saline to promote renal calcium excretion, administration of bisphosphonates or calcitonin to inhibit bone resorption, and addressing underlying causes such as hyperparathyroidism or malignancy. Both conditions require close monitoring of electrolyte levels and cardiac function to prevent life-threatening complications.
Complications and Prognosis
Hyperkalemia can lead to life-threatening cardiac arrhythmias and muscle weakness due to elevated potassium levels disrupting normal cardiac and neuromuscular function. Hypercalcemia poses risks such as kidney stones, bone pain, and neurocognitive disturbances caused by excessive calcium interfering with renal and neurological processes. Prognosis for hyperkalemia often depends on rapid intervention and underlying causes, whereas hypercalcemia prognosis varies based on etiology, with malignancy-associated cases having poorer outcomes.
Prevention and Long-Term Management
Preventing hyperkalemia involves maintaining a potassium-restricted diet, regular monitoring of serum potassium levels in patients with chronic kidney disease, and careful use of medications such as ACE inhibitors or potassium-sparing diuretics. In contrast, hypercalcemia prevention emphasizes adequate hydration, avoiding excessive vitamin D or calcium supplements, and assessing for underlying conditions like hyperparathyroidism. Long-term management of hyperkalemia may require potassium binders and dialysis in advanced cases, while persistent hypercalcemia often necessitates treating the primary cause, such as parathyroidectomy for hyperparathyroidism or bisphosphonates to reduce calcium levels.
Hyperkalemia Infographic
 libterm.com
libterm.com