Hemiparesis is characterized by weakness on one side of the body, often resulting from stroke or brain injury, whereas ataxia involves a lack of muscle coordination affecting balance and movement. Understanding the distinct causes and symptoms of these neurological conditions is essential for effective diagnosis and treatment. Explore the rest of this article to learn how to identify, manage, and address hemiparesis and ataxia for better patient outcomes.
Table of Comparison
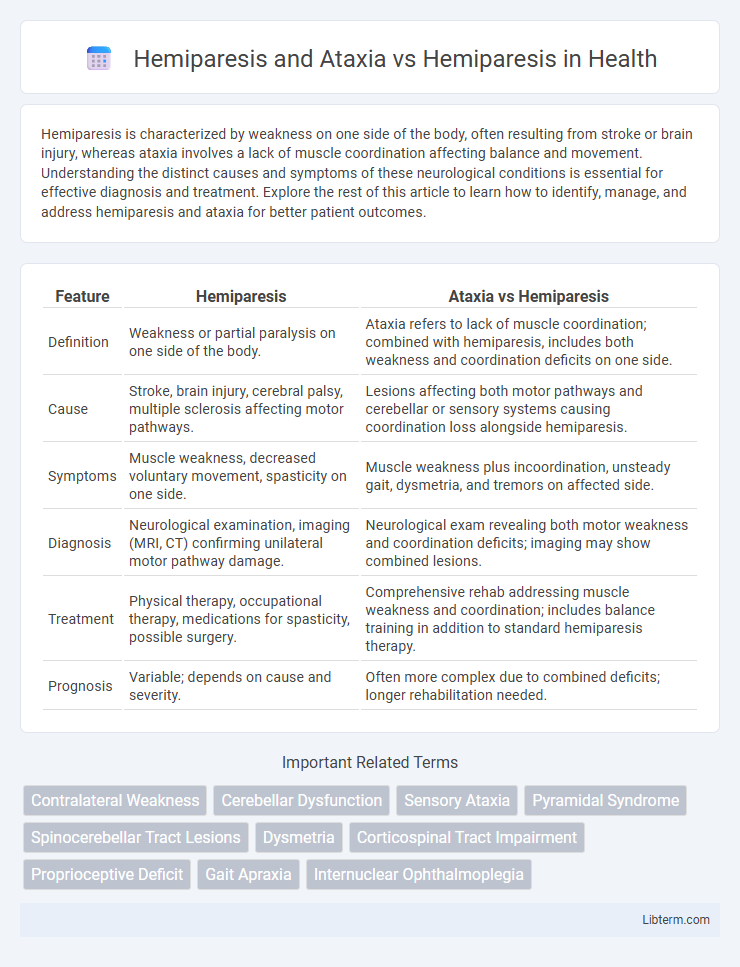
| Feature | Hemiparesis | Ataxia vs Hemiparesis |
|---|---|---|
| Definition | Weakness or partial paralysis on one side of the body. | Ataxia refers to lack of muscle coordination; combined with hemiparesis, includes both weakness and coordination deficits on one side. |
| Cause | Stroke, brain injury, cerebral palsy, multiple sclerosis affecting motor pathways. | Lesions affecting both motor pathways and cerebellar or sensory systems causing coordination loss alongside hemiparesis. |
| Symptoms | Muscle weakness, decreased voluntary movement, spasticity on one side. | Muscle weakness plus incoordination, unsteady gait, dysmetria, and tremors on affected side. |
| Diagnosis | Neurological examination, imaging (MRI, CT) confirming unilateral motor pathway damage. | Neurological exam revealing both motor weakness and coordination deficits; imaging may show combined lesions. |
| Treatment | Physical therapy, occupational therapy, medications for spasticity, possible surgery. | Comprehensive rehab addressing muscle weakness and coordination; includes balance training in addition to standard hemiparesis therapy. |
| Prognosis | Variable; depends on cause and severity. | Often more complex due to combined deficits; longer rehabilitation needed. |
Introduction to Hemiparesis and Ataxia
Hemiparesis and ataxia are neurological conditions that often co-occur but affect motor function differently; hemiparesis involves weakness on one side of the body due to brain or spinal cord injury, while ataxia manifests as impaired coordination and balance caused by cerebellar dysfunction. Understanding the distinct pathophysiology and clinical presentations is critical for accurate diagnosis and targeted rehabilitation strategies. Differentiating hemiparesis combined with ataxia from isolated hemiparesis enables clinicians to address both muscle strength deficits and motor coordination impairments effectively.
Defining Hemiparesis: Causes and Symptoms
Hemiparesis is a neurological condition characterized by weakness or partial paralysis on one side of the body, often caused by stroke, traumatic brain injury, or multiple sclerosis. Symptoms include muscle weakness, impaired motor control, and reduced coordination on the affected side, leading to difficulties in movement and daily activities. While hemiparesis primarily involves weakness, ataxia adds impaired balance and coordination, often resulting from cerebellar dysfunction.
Understanding Ataxia: Key Features and Origins
Ataxia is a neurological condition characterized by impaired coordination, balance, and speech, often resulting from cerebellar dysfunction or damage to neural pathways involved in motor control. Unlike hemiparesis, which involves weakness or partial paralysis on one side of the body due to corticospinal tract lesions, ataxia primarily affects the smooth execution of voluntary movements without muscle weakness. Understanding the origins of ataxia, including cerebellar stroke, multiple sclerosis, or genetic disorders, is crucial for differentiating it from hemiparesis and guiding appropriate treatment strategies.
Hemiparesis vs Hemiparesis with Ataxia: What’s the Difference?
Hemiparesis refers to weakness or partial paralysis on one side of the body, often caused by stroke or brain injury. Hemiparesis with ataxia combines this weakness with ataxia, which involves impaired coordination and balance, resulting from damage to the cerebellum or its pathways. The presence of ataxia alongside hemiparesis indicates a more complex neurological impairment affecting both motor strength and coordination, necessitating tailored rehabilitation strategies.
Neurological Pathways Involved in Both Conditions
Hemiparesis involves unilateral weakness primarily due to lesions in the corticospinal tract affecting motor signal transmission from the cerebral cortex to the spinal cord. Ataxia, when combined with hemiparesis, indicates involvement of the cerebellar pathways responsible for coordination and balance, alongside corticospinal tract damage. The distinction lies in the disruption of the cerebellar afferent and efferent fibers in ataxia, causing impaired proprioceptive integration, while isolated hemiparesis reflects pure motor pathway impairment without cerebellar dysfunction.
Clinical Assessment and Diagnostic Approaches
Clinical assessment of hemiparesis involves detailed neurological examination focusing on muscle strength, tone, reflexes, and sensory deficits, while ataxia evaluation emphasizes coordination, balance, and gait analysis through tests like finger-to-nose and heel-to-shin. Diagnostic approaches for hemiparesis commonly include neuroimaging modalities such as MRI and CT scans to identify underlying lesions like stroke or tumor, whereas ataxia assessment may require electrophysiological studies, genetic testing, and vestibular function tests to pinpoint cerebellar or proprioceptive dysfunction. Differentiating hemiparesis from conditions presenting with hemiparesis and ataxia necessitates a comprehensive approach combining clinical signs with targeted investigations to guide effective management.
Common Underlying Disorders and Conditions
Hemiparesis and ataxia often co-occur in neurological conditions such as stroke, multiple sclerosis, and brain tumors, where damage to both motor and cerebellar pathways affects muscle strength and coordination. In contrast, isolated hemiparesis is primarily associated with conditions that selectively impact the corticospinal tract, including ischemic stroke and localized brain injury. Understanding the overlapping and distinct pathophysiology of these disorders aids in accurate diagnosis and targeted rehabilitation strategies.
Impact on Daily Function and Mobility
Hemiparesis combined with ataxia significantly impairs coordination, balance, and muscle strength, leading to greater challenges in daily activities and mobility than hemiparesis alone. Individuals with both conditions often experience increased difficulty with walking, fine motor tasks, and maintaining posture, which heightens the risk of falls and reduces independence. Rehabilitation efforts must target both motor weakness and coordination deficits to optimize functional recovery and improve quality of life.
Treatment Strategies: Rehabilitation and Therapy Options
Treatment strategies for hemiparesis combined with ataxia prioritize coordinated multidisciplinary rehabilitation, including physical therapy focused on balance training, motor coordination, and strength building to address both muscle weakness and impaired movement control. Occupational therapy enhances fine motor skills and daily living activities, while speech therapy may be necessary for associated dysarthria or swallowing difficulties. In contrast, hemiparesis without ataxia primarily emphasizes muscle strengthening, mobility exercises, and spasticity management through tailored physiotherapy and pharmacologic interventions.
Prognosis and Long-Term Outcomes
Hemiparesis coupled with ataxia often indicates more extensive neurological damage than hemiparesis alone, leading to a more complex prognosis and potentially longer rehabilitation periods. Patients with hemiparesis and ataxia typically experience greater motor coordination challenges and slower recovery of functional independence compared to those with isolated hemiparesis. Long-term outcomes for hemiparesis combined with ataxia frequently involve persistent balance deficits and increased risk of falls, emphasizing the need for specialized physical therapy interventions targeting both muscle strength and coordination.
Hemiparesis and Ataxia Infographic
 libterm.com
libterm.com