Lymphocytic conditions involve the proliferation or activity of lymphocytes, a type of white blood cell essential for immune response. Understanding the role of lymphocytes can help diagnose and manage diseases such as lymphocytic leukemia, lymphoma, and autoimmune disorders. Explore the rest of this article to learn more about how lymphocytic factors impact your health and treatment options.
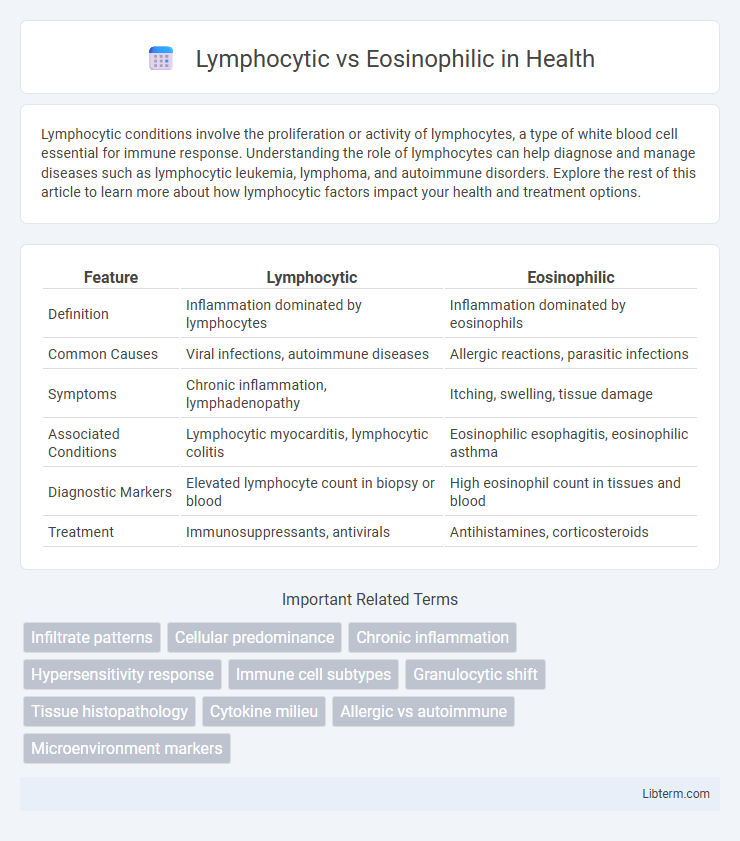
Table of Comparison
| Feature | Lymphocytic | Eosinophilic |
|---|---|---|
| Definition | Inflammation dominated by lymphocytes | Inflammation dominated by eosinophils |
| Common Causes | Viral infections, autoimmune diseases | Allergic reactions, parasitic infections |
| Symptoms | Chronic inflammation, lymphadenopathy | Itching, swelling, tissue damage |
| Associated Conditions | Lymphocytic myocarditis, lymphocytic colitis | Eosinophilic esophagitis, eosinophilic asthma |
| Diagnostic Markers | Elevated lymphocyte count in biopsy or blood | High eosinophil count in tissues and blood |
| Treatment | Immunosuppressants, antivirals | Antihistamines, corticosteroids |
Introduction to Lymphocytic and Eosinophilic Responses
Lymphocytic responses primarily involve lymphocytes, which are crucial for adaptive immunity, targeting specific pathogens through antigen recognition and memory formation. Eosinophilic responses are characterized by the activation and accumulation of eosinophils, cells that play a key role in combating parasitic infections and mediating allergic inflammation. Both responses are integral to the immune system but differ in their cellular effectors and mechanisms of action against various types of threats.
Key Differences Between Lymphocytes and Eosinophils
Lymphocytes primarily function in adaptive immune responses, targeting specific pathogens through antibody production and cytotoxic activity, while eosinophils play a crucial role in combating parasitic infections and mediating allergic reactions by releasing cytotoxic granules. Morphologically, lymphocytes are smaller with a large, round nucleus and scant cytoplasm, whereas eosinophils contain bilobed nuclei and prominent red-orange granules rich in enzymes like major basic protein. Functionally, lymphocytes include B cells, T cells, and natural killer cells integral to immune memory, whereas eosinophils contribute to inflammation and tissue remodeling through their involvement in hypersensitivity and asthma.
Causes of Lymphocytic Infiltration
Lymphocytic infiltration primarily results from chronic infections, autoimmune diseases, and certain cancers, where the immune system activates lymphocytes to target persistent antigens or abnormal cells. Viral infections such as hepatitis C and autoimmune conditions like Hashimoto's thyroiditis frequently trigger lymphocytic infiltration in affected tissues. Unlike eosinophilic infiltration, which is often driven by allergic reactions or parasitic infections, lymphocytic infiltration signifies a sustained immune response involving T and B lymphocytes.
Causes of Eosinophilic Infiltration
Eosinophilic infiltration primarily results from allergic reactions, parasitic infections, and certain autoimmune disorders, with cytokines like IL-5 playing a crucial role in eosinophil activation and recruitment. Lymphocytic infiltration typically arises from viral infections, chronic inflammation, and autoimmune diseases, characterized by T-cell and B-cell accumulation. Understanding the distinct causes of eosinophilic versus lymphocytic infiltration aids in accurate diagnosis and targeted treatment strategies.
Clinical Manifestations: Lymphocytic vs. Eosinophilic Disorders
Lymphocytic disorders often present with symptoms related to chronic inflammation and immune dysregulation, such as persistent fatigue, fever, and lymphadenopathy, reflecting T-cell or B-cell proliferation. Eosinophilic disorders typically manifest with allergic reactions, asthma, skin rashes, and gastrointestinal symptoms like abdominal pain due to eosinophil infiltration and degranulation. Clinical evaluation differentiates these conditions by identifying eosinophilia in blood tests for eosinophilic disorders and lymphocytosis or abnormal lymphocyte morphology in lymphocytic disorders.
Diagnostic Approach and Laboratory Findings
Lymphocytic and eosinophilic disorders are differentiated primarily through targeted diagnostic approaches involving blood tests and tissue biopsy. Lymphocytic conditions typically show elevated lymphocyte counts and specific markers such as CD3 and CD20 on flow cytometry, whereas eosinophilic disorders are characterized by increased eosinophil counts and elevated serum IgE levels. Histopathological examination reveals lymphocyte predominance in lymphocytic disorders and eosinophil infiltration in eosinophilic conditions, aiding precise diagnosis.
Common Diseases Associated with Lymphocytic Predominance
Lymphocytic predominance is commonly associated with chronic viral infections such as hepatitis B and C, as well as autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus. Elevated lymphocyte counts also characterize conditions like lymphocytic leukemia and certain types of lymphoma, including Hodgkin's lymphoma. These diseases typically involve immune system dysregulation, leading to an increase in lymphocyte infiltration and activity in affected tissues.
Common Diseases Associated with Eosinophilic Predominance
Eosinophilic predominance is commonly associated with diseases such as asthma, eosinophilic esophagitis, and certain parasitic infections, where elevated eosinophil levels contribute to inflammation and tissue damage. Conditions like hypereosinophilic syndrome and allergic reactions also exhibit marked eosinophilia, reflecting immune system hyperactivity. Understanding eosinophilic involvement is crucial for diagnosing and managing these disorders, as eosinophils play a key role in allergic and parasitic pathologies.
Treatment Strategies: Lymphocytic vs. Eosinophilic Conditions
Treatment strategies for lymphocytic conditions typically involve immunosuppressive therapies such as corticosteroids and calcineurin inhibitors to reduce lymphocyte infiltration and inflammation. Eosinophilic conditions often require corticosteroids combined with targeted biologics like anti-IL-5 monoclonal antibodies to specifically decrease eosinophil activation and tissue damage. Accurate diagnosis differentiating lymphocytic from eosinophilic pathology ensures tailored treatment, optimizing clinical outcomes and minimizing adverse effects.
Prognosis and Long-term Outcomes
Lymphocytic and eosinophilic inflammation patterns differ significantly in prognosis and long-term outcomes, with lymphocytic conditions often associated with chronic autoimmune diseases that may lead to persistent tissue damage and variable recovery rates. Eosinophilic disorders typically involve allergic or parasitic responses, where prognosis depends on the control of eosinophil-mediated inflammation, with effective treatment leading to better long-term outcomes and reduced risk of organ dysfunction. Understanding the specific inflammatory profile aids in tailoring management strategies, improving disease monitoring, and enhancing quality of life for affected patients.
Lymphocytic Infographic
 libterm.com
libterm.com