Bursitis is the painful inflammation of the bursae, small fluid-filled sacs that cushion bones, tendons, and muscles near joints. This condition often results from repetitive motion or prolonged pressure, leading to swelling, stiffness, and limited joint movement. Discover effective treatments and prevention strategies to protect Your joints in the full article.
Table of Comparison
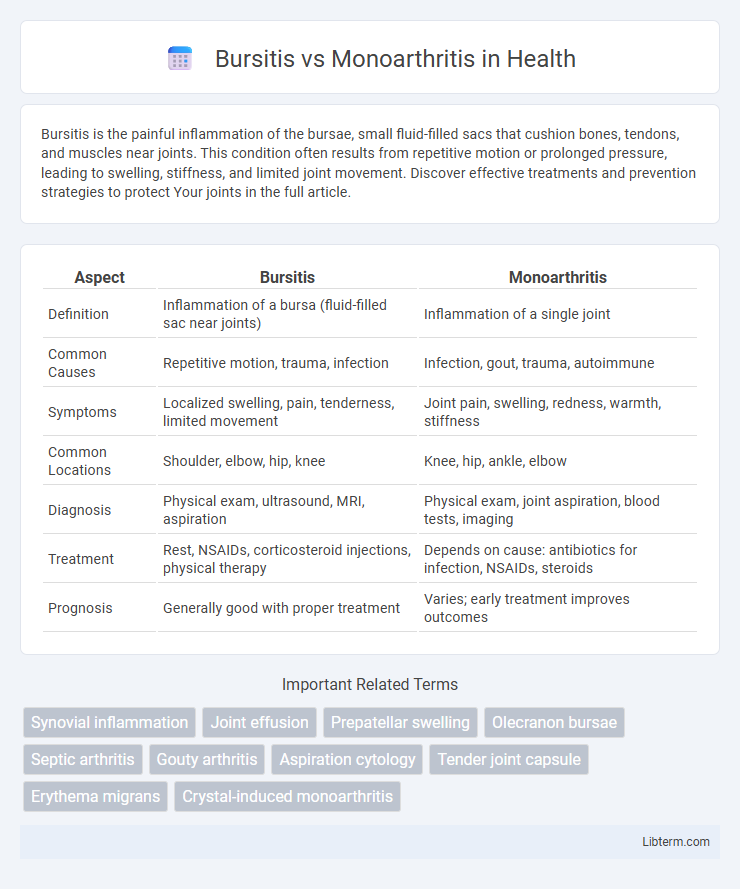
| Aspect | Bursitis | Monoarthritis |
|---|---|---|
| Definition | Inflammation of a bursa (fluid-filled sac near joints) | Inflammation of a single joint |
| Common Causes | Repetitive motion, trauma, infection | Infection, gout, trauma, autoimmune |
| Symptoms | Localized swelling, pain, tenderness, limited movement | Joint pain, swelling, redness, warmth, stiffness |
| Common Locations | Shoulder, elbow, hip, knee | Knee, hip, ankle, elbow |
| Diagnosis | Physical exam, ultrasound, MRI, aspiration | Physical exam, joint aspiration, blood tests, imaging |
| Treatment | Rest, NSAIDs, corticosteroid injections, physical therapy | Depends on cause: antibiotics for infection, NSAIDs, steroids |
| Prognosis | Generally good with proper treatment | Varies; early treatment improves outcomes |
Introduction to Bursitis and Monoarthritis
Bursitis is inflammation of the bursae, small fluid-filled sacs that reduce friction between tissues such as bone, muscle, and tendons, commonly affecting the shoulder, elbow, or hip. Monoarthritis refers to inflammation affecting a single joint, often caused by infection, crystal deposition, or trauma, with symptoms localized to that joint. Understanding the distinct characteristics of bursitis and monoarthritis is essential for accurate diagnosis and targeted treatment.
Understanding Bursitis: Causes and Symptoms
Bursitis is inflammation of the bursa, small fluid-filled sacs that cushion bones, tendons, and muscles near joints, often caused by repetitive motion or injury. Symptoms include localized pain, swelling, tenderness, and limited joint movement, typically affecting shoulder, elbow, hip, or knee. Differentiating bursitis from monoarthritis involves recognizing that monoarthritis usually presents with joint swelling, warmth, and systemic signs from infection or crystal deposition, whereas bursitis primarily affects the soft tissue surrounding the joint.
What is Monoarthritis? Key Features and Triggers
Monoarthritis is characterized by inflammation affecting a single joint, often presenting with swelling, pain, and limited range of motion. Key features include acute onset, redness, warmth, and joint effusion, commonly seen in conditions like gout, septic arthritis, or trauma. Triggers for monoarthritis involve infections, crystal deposition such as urate or calcium pyrophosphate, and direct joint injury, requiring prompt diagnosis to prevent joint damage.
Anatomical Differences: Bursa vs Joint
Bursitis involves inflammation of the bursa, a small fluid-filled sac located between bones, tendons, and muscles to reduce friction, commonly affecting areas like the shoulder, elbow, and knee. Monoarthritis refers to inflammation within a joint capsule itself, typically affecting a single synovial joint such as the knee, hip, or wrist. Anatomically, bursae are extracapsular and serve as cushioning structures, while joints are complex articulations containing cartilage, synovium, and synovial fluid enclosed within a joint capsule.
Risk Factors for Bursitis vs Monoarthritis
Risk factors for bursitis include repetitive joint movements, prolonged pressure on joints, and underlying conditions such as rheumatoid arthritis or gout, which increase inflammation in bursae. Monoarthritis risk factors primarily involve infections like bacterial septic arthritis, crystal-induced arthritis such as gout or pseudogout, and trauma leading to joint inflammation. Identifying these distinct risk factors assists in differential diagnosis and targeted treatment strategies for bursitis versus monoarthritis.
Clinical Presentation: Comparing Signs and Symptoms
Bursitis presents with localized pain, swelling, and tenderness over the affected bursa, often worsening with movement or direct pressure, while monoarthritis typically involves acute onset of joint pain, warmth, swelling, and limited range of motion in a single joint. In bursitis, the surrounding skin usually appears normal without significant erythema, contrasting with monoarthritis, where redness and systemic symptoms like fever may be present, especially in infectious cases. Both conditions cause joint discomfort, but bursitis pain is more superficial and linked to bursa inflammation, whereas monoarthritis reflects intra-articular inflammation affecting the joint space itself.
Diagnostic Approaches: Differentiating Bursitis from Monoarthritis
Diagnostic approaches for differentiating bursitis from monoarthritis rely on clinical evaluation, imaging, and laboratory tests. Ultrasound and MRI effectively identify fluid accumulation and inflammation specific to bursae in bursitis, while joint aspiration with synovial fluid analysis is critical for confirming monoarthritis by detecting infection, crystals, or inflammatory markers. Blood tests measuring inflammatory markers such as ESR and CRP aid in distinguishing systemic inflammatory monoarthritis from localized bursitis.
Treatment Strategies for Bursitis
Treatment strategies for bursitis primarily include rest, ice application, and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. Physical therapy exercises aimed at improving joint function and preventing stiffness are often recommended, alongside corticosteroid injections in severe cases. Unlike monoarthritis, where targeted infection control or disease-specific management is critical, bursitis treatment emphasizes symptom relief and avoiding repetitive joint stress.
Management Options for Monoarthritis
Management options for monoarthritis primarily depend on the underlying cause but typically include anti-inflammatory medications such as NSAIDs to reduce pain and swelling. Joint aspiration may be performed for both diagnostic and therapeutic purposes, particularly in cases of septic arthritis or crystal-induced arthritis, followed by appropriate antibiotic or corticosteroid therapy. Physical therapy and immobilization can help restore joint function and prevent stiffness during the recovery phase.
Prevention and Long-term Outlook
Preventing bursitis involves avoiding repetitive joint stress, using protective gear during physical activities, and maintaining good posture to reduce inflammation risks. Monoarthritis prevention focuses on managing underlying causes like infections or autoimmune diseases through early diagnosis and appropriate treatments such as antibiotics or immunosuppressants. Both conditions benefit from prompt medical intervention to minimize joint damage, with long-term outlooks improving significantly when inflammation is controlled and lifestyle modifications are adopted.
Bursitis Infographic
 libterm.com
libterm.com