Pulmonary edema occurs when fluid accumulates in the lungs, impairing gas exchange and causing difficulty breathing. Common causes include heart failure, acute respiratory distress syndrome, and high-altitude exposure. Discover more about the symptoms, treatment options, and how to manage your condition effectively by reading the rest of the article.
Table of Comparison
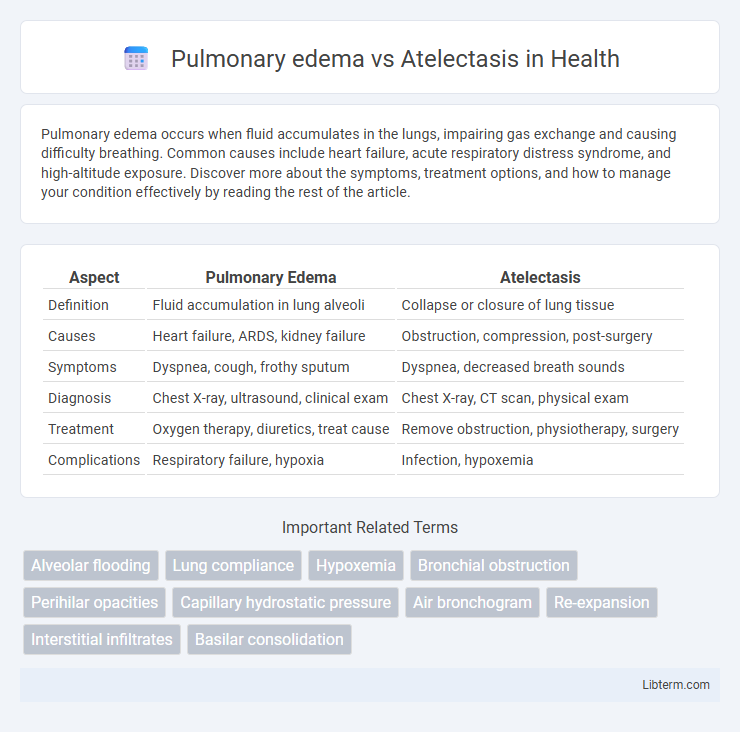
| Aspect | Pulmonary Edema | Atelectasis |
|---|---|---|
| Definition | Fluid accumulation in lung alveoli | Collapse or closure of lung tissue |
| Causes | Heart failure, ARDS, kidney failure | Obstruction, compression, post-surgery |
| Symptoms | Dyspnea, cough, frothy sputum | Dyspnea, decreased breath sounds |
| Diagnosis | Chest X-ray, ultrasound, clinical exam | Chest X-ray, CT scan, physical exam |
| Treatment | Oxygen therapy, diuretics, treat cause | Remove obstruction, physiotherapy, surgery |
| Complications | Respiratory failure, hypoxia | Infection, hypoxemia |
Definition of Pulmonary Edema
Pulmonary edema is a medical condition characterized by the accumulation of excess fluid in the alveoli and interstitial spaces of the lungs, impairing gas exchange and leading to respiratory distress. This condition often results from heart failure, acute respiratory distress syndrome (ARDS), or direct lung injury, causing fluid leakage from the pulmonary capillaries into lung tissues. Unlike atelectasis, which involves the collapse of lung tissue and loss of lung volume, pulmonary edema primarily involves fluid overload and swelling within the lungs.
Definition of Atelectasis
Atelectasis is the complete or partial collapse of a lung or a section (lobe) of a lung, resulting in reduced or absent gas exchange in the affected area. It is caused by obstruction of the airways, pressure from outside the lung, or surfactant deficiency, leading to alveolar collapse. Pulmonary edema, in contrast, involves fluid accumulation within the alveoli and interstitial spaces, impairing oxygen diffusion rather than lung collapse.
Etiology: Causes of Pulmonary Edema
Pulmonary edema primarily results from left ventricular heart failure, which leads to increased hydrostatic pressure in pulmonary capillaries causing fluid leakage into alveoli. Other causes include acute respiratory distress syndrome (ARDS), high-altitude exposure, kidney failure causing fluid retention, and inhalation of toxic substances that damage the alveolar-capillary membrane. Non-cardiogenic pulmonary edema arises from increased capillary permeability due to infections, trauma, or allergic reactions.
Etiology: Causes of Atelectasis
Atelectasis primarily results from airway obstruction due to mucus plugs, foreign bodies, or tumors, leading to alveolar collapse and impaired gas exchange. Other causes include compression from pleural effusion, pneumothorax, or lung tumors that restrict lung expansion. Postoperative factors such as shallow breathing and prolonged bed rest also contribute by reducing lung expansion and promoting alveolar collapse.
Clinical Presentation: Signs and Symptoms
Pulmonary edema presents with acute dyspnea, orthopnea, and pink, frothy sputum, accompanied by fine crackles on lung auscultation and possible cyanosis. Atelectasis typically manifests as dyspnea, decreased breath sounds, dullness to percussion, and reduced chest expansion over the affected area. Both conditions may show tachypnea and hypoxemia, but pulmonary edema often involves signs of fluid overload, whereas atelectasis is linked to lung collapse and impaired ventilation.
Radiological Findings and Diagnosis
Pulmonary edema presents radiologically with bilateral, symmetrical perihilar opacities often described as "bat-wing" patterns, accompanied by Kerley B lines and cardiomegaly. Atelectasis appears as area-specific lung volume loss, showing increased opacity, displacement of fissures, ipsilateral mediastinal shift, or elevation of the diaphragm on chest X-rays or CT scans. Diagnosis of pulmonary edema relies on imaging combined with clinical signs of fluid overload and cardiac dysfunction, whereas atelectasis diagnosis emphasizes identifying localized lung collapse without vascular congestion.
Pathophysiology: Underlying Mechanisms
Pulmonary edema results from increased hydrostatic pressure or increased capillary permeability causing fluid accumulation within the alveoli and interstitial spaces, impairing gas exchange. Atelectasis occurs due to alveolar collapse caused by airway obstruction, surfactant deficiency, or external compression, leading to reduced lung volume and ventilation-perfusion mismatch. Both conditions disrupt normal alveolar function but differ in the origin of alveolar impairment: fluid accumulation in pulmonary edema versus loss of alveolar air in atelectasis.
Treatment Approaches for Pulmonary Edema
Treatment for pulmonary edema primarily involves addressing the underlying cause, such as heart failure, by using diuretics like furosemide to reduce fluid overload and supplemental oxygen to improve hypoxia. Positive pressure ventilation, including CPAP or mechanical ventilation, may be necessary in severe cases to maintain adequate oxygenation and alveolar patency. Management differs from atelectasis, where treatments typically focus on airway clearance techniques, lung expansion exercises, and sometimes bronchoscopy to remove obstructions.
Treatment Approaches for Atelectasis
Treatment approaches for atelectasis typically involve techniques to re-expand the collapsed lung tissue and improve ventilation, such as incentive spirometry, chest physiotherapy, and deep breathing exercises. Non-invasive methods like positive airway pressure therapies, including CPAP or BiPAP, may be used to maintain airway patency and prevent alveolar collapse. In severe cases, bronchoscopy can be employed to remove mucous plugs or obstructions that contribute to atelectasis.
Key Differences and Clinical Implications
Pulmonary edema involves fluid accumulation in the alveoli, causing impaired gas exchange and decreased lung compliance, while atelectasis is characterized by alveolar collapse leading to reduced lung volume and ventilation-perfusion mismatch. Clinically, pulmonary edema presents with symptoms like dyspnea, crackles on auscultation, and hypoxemia due to fluid overload or cardiac failure, whereas atelectasis often results from airway obstruction or postoperative complications, manifesting as diminished breath sounds and potentially fever. Treatment for pulmonary edema focuses on diuretics and addressing cardiac function, while atelectasis management includes airway clearance techniques, bronchodilators, and encouraging deep breathing exercises to re-expand collapsed lung tissue.
Pulmonary edema Infographic
 libterm.com
libterm.com