Gastroparesis is a condition where the stomach empties slowly due to nerve damage, while intestinal obstruction involves a blockage that prevents the normal flow of digestive contents through the intestines. Both conditions can cause severe abdominal discomfort, bloating, nausea, and vomiting, requiring prompt medical diagnosis and management to avoid complications. To understand more about these digestive disorders and how they affect Your health, continue reading the rest of the article.
Table of Comparison
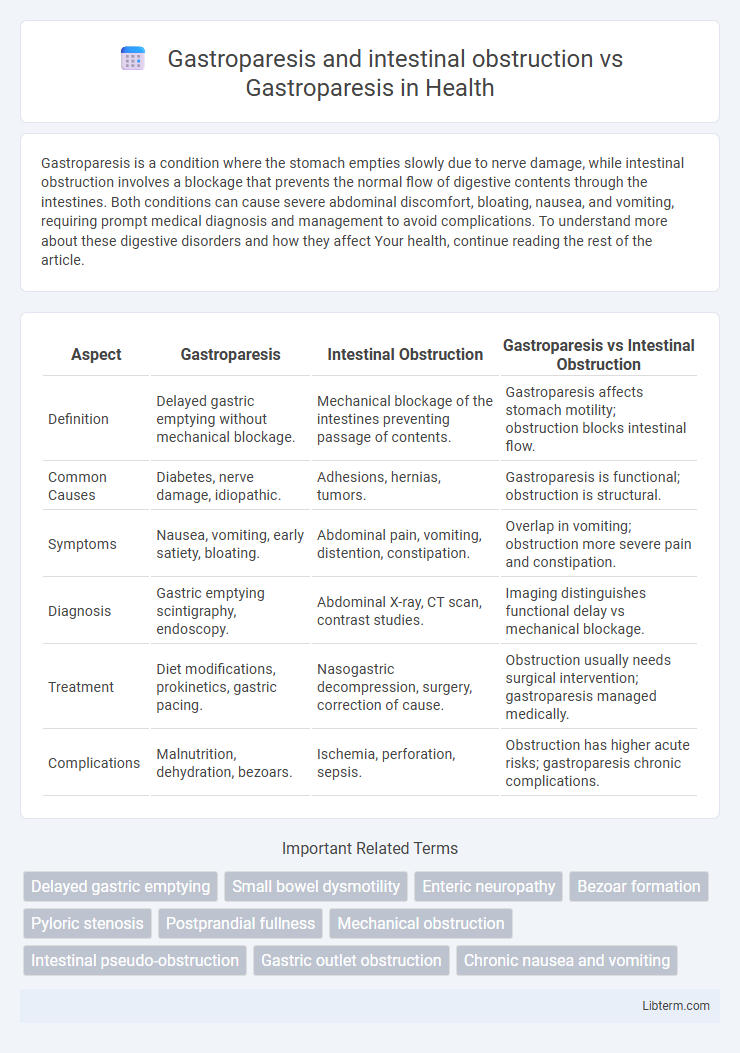
| Aspect | Gastroparesis | Intestinal Obstruction | Gastroparesis vs Intestinal Obstruction |
|---|---|---|---|
| Definition | Delayed gastric emptying without mechanical blockage. | Mechanical blockage of the intestines preventing passage of contents. | Gastroparesis affects stomach motility; obstruction blocks intestinal flow. |
| Common Causes | Diabetes, nerve damage, idiopathic. | Adhesions, hernias, tumors. | Gastroparesis is functional; obstruction is structural. |
| Symptoms | Nausea, vomiting, early satiety, bloating. | Abdominal pain, vomiting, distention, constipation. | Overlap in vomiting; obstruction more severe pain and constipation. |
| Diagnosis | Gastric emptying scintigraphy, endoscopy. | Abdominal X-ray, CT scan, contrast studies. | Imaging distinguishes functional delay vs mechanical blockage. |
| Treatment | Diet modifications, prokinetics, gastric pacing. | Nasogastric decompression, surgery, correction of cause. | Obstruction usually needs surgical intervention; gastroparesis managed medically. |
| Complications | Malnutrition, dehydration, bezoars. | Ischemia, perforation, sepsis. | Obstruction has higher acute risks; gastroparesis chronic complications. |
Understanding Gastroparesis: Definition and Causes
Gastroparesis is a chronic disorder characterized by delayed gastric emptying without mechanical obstruction, often caused by diabetes, viral infections, or nerve damage. Intestinal obstruction involves a physical blockage in the intestines that impedes the passage of contents, which contrasts with gastroparesis's motility impairment. Understanding gastroparesis requires recognizing its distinct pathophysiology from obstructions, focusing on neuromuscular dysfunction rather than mechanical blockage.
What is Intestinal Obstruction? Key Differences from Gastroparesis
Intestinal obstruction is a blockage preventing the normal flow of contents through the intestines, often caused by adhesions, hernias, or tumors, leading to severe abdominal pain, vomiting, and constipation. Gastroparesis is a condition characterized by delayed stomach emptying due to nerve dysfunction without physical blockage, causing symptoms like nausea, bloating, and early satiety. Unlike gastroparesis, intestinal obstruction is a mechanical or functional barrier requiring urgent medical or surgical intervention to restore bowel passage.
Gastroparesis vs Intestinal Obstruction: Core Symptoms Compared
Gastroparesis is characterized by delayed gastric emptying causing nausea, vomiting, early satiety, and bloating, whereas intestinal obstruction primarily presents with severe abdominal pain, distension, vomiting, and constipation due to a physical blockage in the intestines. Core symptoms of gastroparesis reflect impaired gastric motility without mechanical obstruction, while intestinal obstruction symptoms indicate a critical, often acute, disruption to bowel continuity. Differentiating these conditions involves imaging studies like gastric emptying scans for gastroparesis and abdominal X-rays or CT scans to identify obstruction sites.
Diagnostic Approaches for Gastroparesis
Diagnostic approaches for gastroparesis primarily involve gastric emptying studies such as scintigraphy, which measures the rate at which food leaves the stomach, distinguishing delayed gastric emptying from normal function. Imaging modalities like abdominal X-rays or CT scans help rule out intestinal obstruction by visualizing mechanical blockages, a key factor differentiating gastroparesis from obstruction-related symptoms. Endoscopic evaluations and gastric manometry provide additional insights into gastric motility disorders, enhancing diagnostic accuracy for gastroparesis.
Diagnostic Strategies to Identify Intestinal Obstruction
Diagnostic strategies to identify intestinal obstruction in patients with gastroparesis prioritize imaging techniques such as abdominal X-rays, CT scans, and MRI to detect mechanical blockages. Endoscopic evaluation and contrast studies, like a gastrografin enema, further delineate the location and severity of obstruction, differentiating it from delayed gastric emptying due to gastroparesis alone. Biomarkers and motility tests remain essential but must be interpreted alongside imaging to accurately distinguish between functional gastroparesis and true intestinal obstruction.
Overlapping Symptoms: Challenges in Differentiation
Gastroparesis and intestinal obstruction share overlapping symptoms such as nausea, vomiting, abdominal pain, and bloating, complicating accurate diagnosis. Both conditions can impair gastric motility, leading to delayed gastric emptying and similar clinical presentations. Differentiating requires targeted diagnostic tools like gastric emptying studies for gastroparesis and imaging techniques such as abdominal X-rays or CT scans to identify obstructions.
Imaging and Testing: Distinguishing Between Conditions
Imaging plays a critical role in differentiating gastroparesis from intestinal obstruction, with gastric emptying studies and scintigraphy used primarily to assess delayed gastric motility in gastroparesis. Abdominal X-rays, CT scans, and contrast studies help identify mechanical blockages, bowel dilation, or transition points indicative of intestinal obstruction. Combining functional tests for gastric motility with structural imaging enables accurate diagnosis and guides tailored management strategies.
Treatment Options for Gastroparesis
Treatment options for gastroparesis primarily include dietary modifications such as small, frequent meals low in fat and fiber, prokinetic medications like metoclopramide to enhance gastric motility, and antiemetics to control nausea. In severe cases unresponsive to medical therapy, interventions such as gastric electrical stimulation or, rarely, surgical procedures like pyloroplasty may be considered. Intestinal obstruction requires distinct management, often necessitating surgical intervention or decompression, which contrasts with the primarily medical and dietary focus in gastroparesis treatment.
Management Strategies for Intestinal Obstruction
Management strategies for intestinal obstruction in patients with gastroparesis prioritize prompt decompression of the gastrointestinal tract using nasogastric suctioning or endoscopic interventions to relieve symptoms and prevent complications. Surgical consultation is essential for cases where obstruction is complete, refractory, or complicated by ischemia, while conservative approaches including bowel rest, intravenous fluids, and electrolyte correction are implemented for partial obstructions. Pharmacologic therapy targeting underlying gastroparesis, such as prokinetics, may be adjusted but are contraindicated during acute obstruction until resolution.
Prognosis and Patient Outcomes: Gastroparesis vs Intestinal Obstruction
Gastroparesis typically presents with chronic delayed gastric emptying leading to symptoms like nausea, vomiting, and malnutrition, with a prognosis often involving long-term symptom management and variable quality of life outcomes. Intestinal obstruction, in contrast, is an acute surgical emergency with risks of bowel ischemia and perforation; without prompt intervention, it carries a high morbidity and mortality rate. While gastroparesis patients may experience fluctuating symptom control and nutritional challenges, those with intestinal obstruction require immediate treatment to prevent life-threatening complications, resulting in distinctly different patient outcomes and prognostic trajectories.
Gastroparesis and intestinal obstruction Infographic
 libterm.com
libterm.com