Encephalitis is a serious inflammation of the brain usually caused by viral infections, leading to symptoms such as headache, fever, confusion, and seizures. Prompt diagnosis and treatment are crucial to reduce the risk of long-term neurological damage and improve recovery outcomes. Discover more about the causes, symptoms, and effective treatment options in the rest of this article.
Table of Comparison
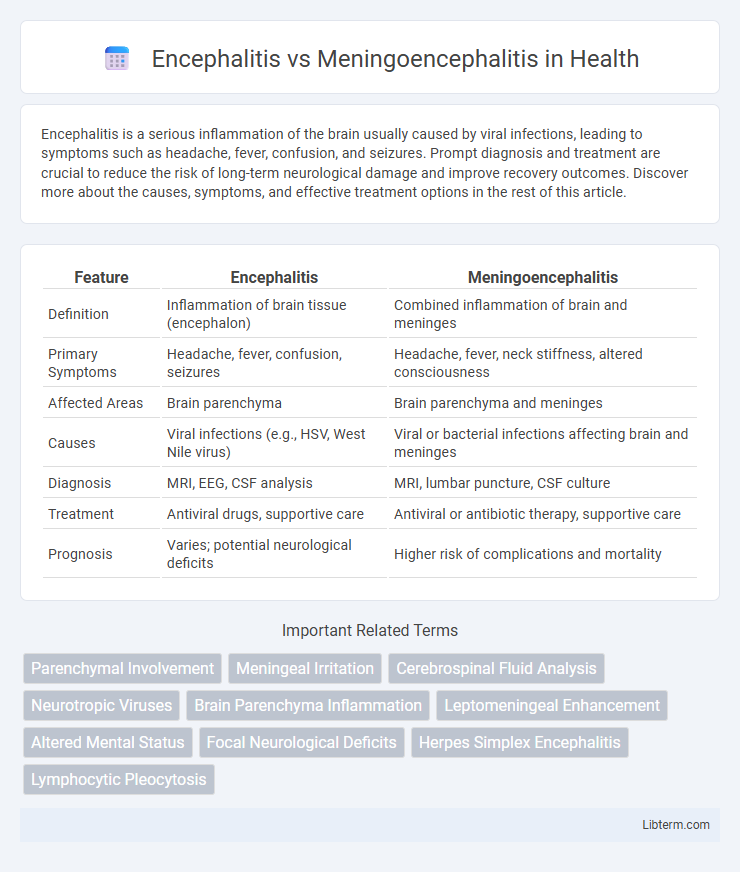
| Feature | Encephalitis | Meningoencephalitis |
|---|---|---|
| Definition | Inflammation of brain tissue (encephalon) | Combined inflammation of brain and meninges |
| Primary Symptoms | Headache, fever, confusion, seizures | Headache, fever, neck stiffness, altered consciousness |
| Affected Areas | Brain parenchyma | Brain parenchyma and meninges |
| Causes | Viral infections (e.g., HSV, West Nile virus) | Viral or bacterial infections affecting brain and meninges |
| Diagnosis | MRI, EEG, CSF analysis | MRI, lumbar puncture, CSF culture |
| Treatment | Antiviral drugs, supportive care | Antiviral or antibiotic therapy, supportive care |
| Prognosis | Varies; potential neurological deficits | Higher risk of complications and mortality |
Introduction to Encephalitis and Meningoencephalitis
Encephalitis is an inflammation of the brain tissue typically caused by viral infections such as herpes simplex virus, leading to symptoms like fever, headache, and altered mental status. Meningoencephalitis combines inflammation of both the brain (encephalitis) and the meninges, the protective membranes surrounding the brain and spinal cord, often resulting from infections like bacterial, viral, or fungal agents. Differentiating encephalitis from meningoencephalitis is critical due to overlapping symptoms but requires distinct diagnostic approaches including cerebrospinal fluid analysis and neuroimaging to guide targeted treatment strategies.
Definitions and Key Differences
Encephalitis refers to the inflammation of the brain tissue, primarily caused by viral infections or autoimmune responses. Meningoencephalitis involves the simultaneous inflammation of both the brain (encephalitis) and the meninges, the protective membranes covering the brain and spinal cord. Key differences include the broader symptom range and increased severity in meningoencephalitis, often requiring more intensive diagnostic and therapeutic approaches.
Causes and Risk Factors
Encephalitis primarily results from viral infections such as herpes simplex virus, West Nile virus, and enteroviruses, whereas meningoencephalitis involves inflammation of both the brain and meninges typically caused by bacterial, viral, or fungal infections like Neisseria meningitidis, herpes simplex virus, and Cryptococcus neoformans. Risk factors for encephalitis include young age, immunosuppression, and exposure to insect vectors, while meningoencephalitis risk increases with immune deficiencies, recent infections, and close contact settings. Understanding these differences in causative agents and predisposing conditions is crucial for accurate diagnosis and targeted treatment strategies.
Pathophysiology and Disease Mechanisms
Encephalitis involves inflammation of the brain parenchyma primarily due to viral infections, leading to neuronal damage and disrupted neurotransmission. Meningoencephalitis combines inflammation of both the brain parenchyma and meninges, resulting in a more extensive immune response with increased blood-brain barrier permeability and cerebrospinal fluid abnormalities. The overlapping pathophysiology includes viral entry through hematogenous spread or direct neural invasion, triggering cytokine release, glial activation, and resultant neurotoxicity.
Clinical Symptoms and Presentation
Encephalitis typically presents with altered mental status, seizures, and focal neurological deficits, reflecting inflammation primarily of the brain parenchyma. Meningoencephalitis combines these brain symptoms with meningeal signs such as neck stiffness, photophobia, and headache, indicating concurrent inflammation of both the meninges and brain tissue. Fever, confusion, and lethargy are common in both conditions but are often more pronounced in meningoencephalitis due to widespread CNS involvement.
Diagnostic Approaches and Laboratory Findings
Diagnostic approaches for encephalitis primarily include brain imaging such as MRI to detect inflammation, lumbar puncture for cerebrospinal fluid (CSF) analysis, and polymerase chain reaction (PCR) testing to identify viral pathogens. Meningoencephalitis diagnosis integrates similar methods but places greater emphasis on CSF analysis showing pleocytosis, elevated protein, and sometimes decreased glucose indicating both meningeal and brain involvement. Laboratory findings in meningoencephalitis often reveal a mixed inflammatory response with elevated white blood cells and viral or bacterial markers, distinguishing it from isolated encephalitis which may display more confined neurological inflammation.
Imaging and Radiological Features
Encephalitis typically presents with MRI showing hyperintense lesions on T2-weighted and FLAIR sequences, often involving the temporal lobes, whereas meningoencephalitis demonstrates combined features of both meningeal enhancement and parenchymal inflammation. Contrast-enhanced MRI reveals leptomeningeal enhancement in meningoencephalitis, reflecting meningeal involvement absent in isolated encephalitis. Diffusion-weighted imaging (DWI) may show restricted diffusion in affected areas, aiding differentiation and assessment of disease severity.
Treatment Options and Management
Treatment options for encephalitis primarily include antiviral medications such as acyclovir for herpes simplex virus, supportive care to manage symptoms, and corticosteroids in select cases to reduce inflammation. In meningoencephalitis, management combines therapies targeting both meningitis and encephalitis, often involving broad-spectrum antibiotics to combat bacterial infections, antivirals where viral causes are suspected, and supportive measures like seizure control and intracranial pressure monitoring. Early diagnosis and tailored treatment protocols significantly improve patient outcomes in both encephalitis and meningoencephalitis.
Prognosis and Potential Complications
Encephalitis, characterized by brain inflammation, typically presents with neurological deficits that can range from mild to severe, influencing prognosis based on the causative agent and timeliness of treatment. Meningoencephalitis, involving inflammation of both the brain and meninges, carries a higher risk of complications such as seizures, cognitive impairment, and long-term neurological dysfunction due to combined tissue involvement. Early diagnosis and intervention are critical in both conditions to minimize complications, with meningoencephalitis generally associated with a more guarded prognosis due to its dual impact on central nervous system structures.
Prevention Strategies and Public Health Implications
Effective prevention strategies for encephalitis and meningoencephalitis primarily include vaccination against causative agents such as Japanese encephalitis virus, measles, mumps, and rubella virus, alongside vector control measures targeting mosquitoes to reduce transmission. Public health implications emphasize the need for widespread immunization programs, enhanced surveillance systems for early outbreak detection, and public education campaigns to minimize infection risks and improve healthcare response. Implementing integrated preventative approaches reduces morbidity and mortality associated with neuroinflammatory diseases, ultimately preserving community health and reducing healthcare costs.
Encephalitis Infographic
 libterm.com
libterm.com