Fibrillation refers to rapid, irregular contractions of muscle fibers, most commonly affecting the heart's atria or ventricles. This condition disrupts normal heart rhythms, potentially leading to complications such as stroke or heart failure if untreated. Explore the rest of this article to understand how fibrillation impacts your health and the available treatment options.
Table of Comparison
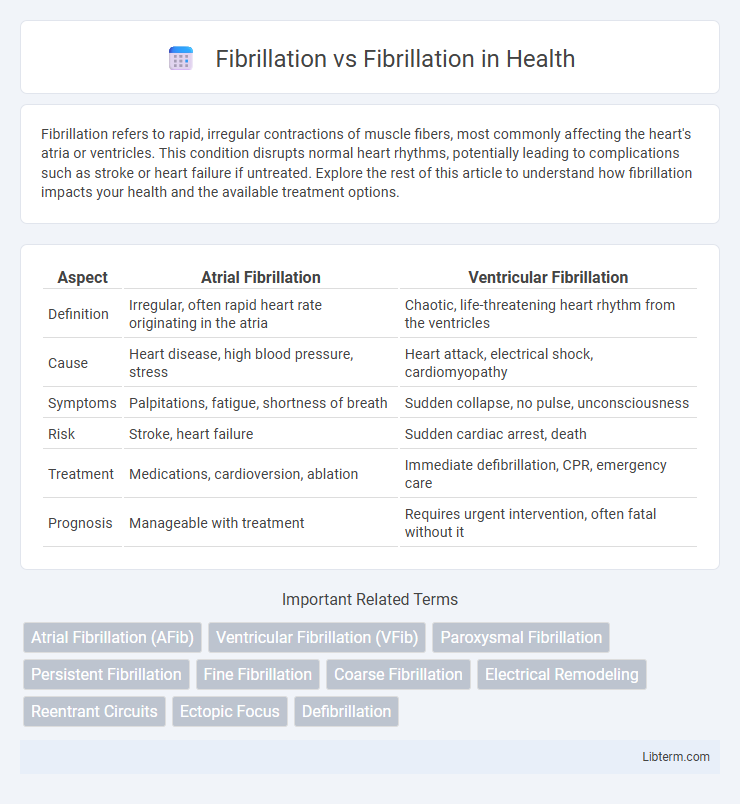
| Aspect | Atrial Fibrillation | Ventricular Fibrillation |
|---|---|---|
| Definition | Irregular, often rapid heart rate originating in the atria | Chaotic, life-threatening heart rhythm from the ventricles |
| Cause | Heart disease, high blood pressure, stress | Heart attack, electrical shock, cardiomyopathy |
| Symptoms | Palpitations, fatigue, shortness of breath | Sudden collapse, no pulse, unconsciousness |
| Risk | Stroke, heart failure | Sudden cardiac arrest, death |
| Treatment | Medications, cardioversion, ablation | Immediate defibrillation, CPR, emergency care |
| Prognosis | Manageable with treatment | Requires urgent intervention, often fatal without it |
Understanding Fibrillation: Definition and Types
Fibrillation refers to rapid, irregular heart muscle contractions disrupting normal cardiac rhythm, primarily classified into atrial fibrillation and ventricular fibrillation. Atrial fibrillation involves disorganized electrical activity in the atria, leading to inefficient blood flow and increased stroke risk, while ventricular fibrillation causes chaotic impulses in the ventricles, often resulting in sudden cardiac arrest if untreated. Recognizing the differences between these fibrillation types is critical for diagnosis, treatment selection, and improving patient outcomes in cardiovascular care.
Atrial Fibrillation vs Ventricular Fibrillation: Key Differences
Atrial fibrillation (AFib) is characterized by rapid, irregular beating of the atria, leading to inefficient blood flow and increased stroke risk, whereas ventricular fibrillation (VFib) involves erratic electrical activity in the ventricles, causing the heart to quiver instead of pumping blood effectively, which is immediately life-threatening. AFib often results from conditions like hypertension or heart valve disease and may cause palpitations, fatigue, or no symptoms, while VFib typically occurs during heart attacks and requires urgent defibrillation for survival. The management of AFib includes anticoagulation and rate control, whereas VFib demands emergency CPR and defibrillation to restore a viable heart rhythm.
Causes of Fibrillation: Common Risk Factors
Fibrillation, including atrial fibrillation and ventricular fibrillation, arises primarily from abnormalities in the heart's electrical signals, often triggered by high blood pressure, coronary artery disease, and heart valve disorders. Common risk factors include advanced age, obesity, excessive alcohol consumption, and a history of heart attacks or heart failure. Understanding these causes is crucial for preventing and managing fibrillation to reduce stroke and sudden cardiac arrest risks.
Symptoms: How Fibrillation Manifests
Fibrillation manifests through irregular and often rapid heartbeats, leading to symptoms such as palpitations, dizziness, fatigue, and shortness of breath. Atrial fibrillation specifically causes an erratic atrial rhythm, increasing the risk of stroke, while ventricular fibrillation results in disorganized ventricular contractions that can cause sudden cardiac arrest. Recognizing these distinct symptoms is crucial for timely diagnosis and treatment to prevent severe complications.
Pathophysiology: What Happens in the Heart
Atrial fibrillation and ventricular fibrillation both involve disorganized electrical activity in the heart, disrupting normal rhythm. In atrial fibrillation, rapid and irregular impulses in the atria cause ineffective atrial contractions, reducing cardiac output and increasing stroke risk due to blood pooling. Ventricular fibrillation results from chaotic electrical signals in the ventricles, leading to inability to pump blood effectively and causing sudden cardiac arrest if not promptly treated.
Diagnosis: How Fibrillation is Detected
Fibrillation is detected primarily through electrocardiogram (ECG) recordings, which reveal irregular, rapid electrical impulses indicative of atrial or ventricular fibrillation. Holter monitors or event recorders provide extended heart rhythm monitoring to capture intermittent fibrillation episodes often missed in standard ECGs. Advanced diagnostic tools like intracardiac electrophysiology studies help pinpoint the exact fibrillation source for targeted treatment.
Complications Associated with Fibrillation
Complications associated with fibrillation primarily include an increased risk of stroke due to the formation of blood clots in the atria, which can embolize to the brain. Heart failure commonly develops as a result of the irregular and often rapid heart rate impairing effective cardiac output. Other risks include chronic fatigue and a heightened chance of developing persistent arrhythmias, which compromise overall cardiovascular health.
Treatment Options for Different Types of Fibrillation
Treatment options for atrial fibrillation typically include rate control medications such as beta-blockers, rhythm control strategies using antiarrhythmic drugs, and anticoagulants to reduce stroke risk. Ventricular fibrillation requires immediate defibrillation with an automated external defibrillator (AED) and advanced cardiac life support measures, often followed by implantable cardioverter-defibrillator (ICD) placement. Catheter ablation may be used in recurrent atrial fibrillation cases to restore normal heart rhythm and improve quality of life.
Prevention and Lifestyle Modifications
Preventing fibrillation, particularly atrial fibrillation, involves managing risk factors such as high blood pressure, obesity, and sleep apnea through lifestyle modifications like regular physical activity, a heart-healthy diet rich in fruits and vegetables, and stress reduction techniques. Limiting alcohol intake and avoiding tobacco use significantly reduce the likelihood of developing fibrillation by improving overall cardiovascular health. Consistent monitoring and controlling underlying conditions like diabetes and thyroid disorders further aid in fibrillation prevention and promote long-term heart rhythm stability.
Prognosis: Outcomes and Long-Term Management
Atrial fibrillation and ventricular fibrillation differ significantly in prognosis and long-term management. Atrial fibrillation often requires anticoagulation therapy to reduce stroke risk and may be managed with rate or rhythm control strategies, contributing to a variable but generally manageable long-term outlook. Ventricular fibrillation, associated with sudden cardiac arrest, demands immediate defibrillation and advanced cardiac life support; survivors usually need implantable cardioverter-defibrillators and aggressive risk factor modification to improve survival rates.
Fibrillation Infographic
 libterm.com
libterm.com