Pancytopenia is a medical condition characterized by a reduction in red and white blood cells, as well as platelets, leading to symptoms such as fatigue, increased infections, and bleeding tendencies. This complex disorder can result from various causes including bone marrow failure, certain infections, autoimmune diseases, or exposure to toxins. To understand the symptoms, causes, and treatment options for your health, continue reading the rest of the article.
Table of Comparison
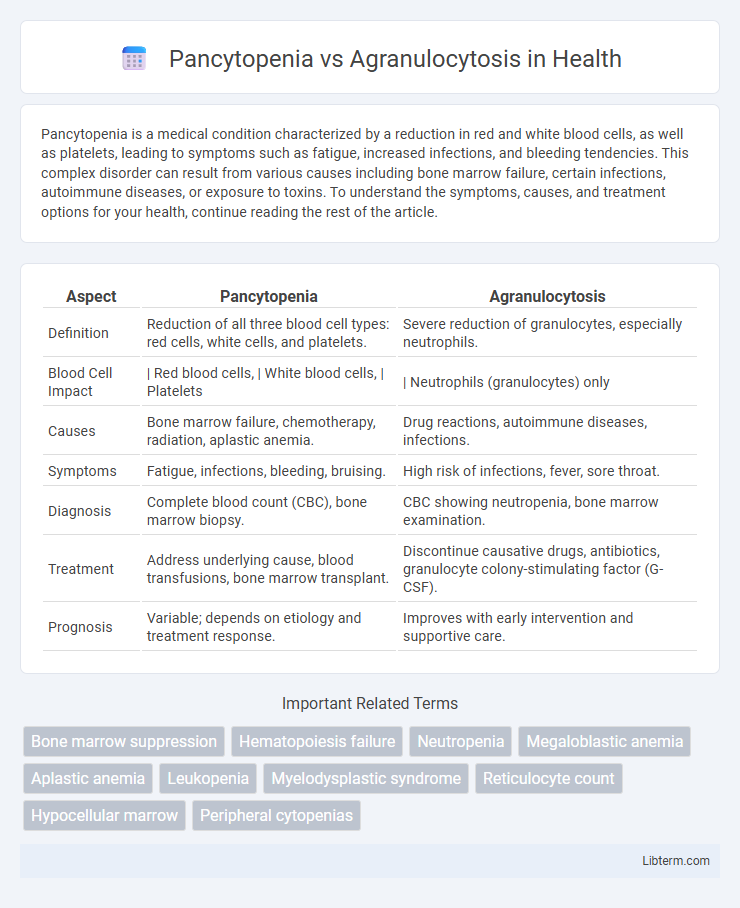
| Aspect | Pancytopenia | Agranulocytosis |
|---|---|---|
| Definition | Reduction of all three blood cell types: red cells, white cells, and platelets. | Severe reduction of granulocytes, especially neutrophils. |
| Blood Cell Impact | | Red blood cells, | White blood cells, | Platelets | | Neutrophils (granulocytes) only |
| Causes | Bone marrow failure, chemotherapy, radiation, aplastic anemia. | Drug reactions, autoimmune diseases, infections. |
| Symptoms | Fatigue, infections, bleeding, bruising. | High risk of infections, fever, sore throat. |
| Diagnosis | Complete blood count (CBC), bone marrow biopsy. | CBC showing neutropenia, bone marrow examination. |
| Treatment | Address underlying cause, blood transfusions, bone marrow transplant. | Discontinue causative drugs, antibiotics, granulocyte colony-stimulating factor (G-CSF). |
| Prognosis | Variable; depends on etiology and treatment response. | Improves with early intervention and supportive care. |
Introduction to Pancytopenia and Agranulocytosis
Pancytopenia is a hematological condition characterized by the reduction of all three blood cell types: red blood cells, white blood cells, and platelets, often caused by bone marrow failure or infiltration. Agranulocytosis specifically refers to a severe decrease in granulocytes, particularly neutrophils, leading to increased susceptibility to infections. Both conditions involve compromised immune function but differ in the range and severity of blood cell deficiencies.
Definition of Pancytopenia
Pancytopenia is a hematological condition characterized by the reduction of all three blood cell lines: red blood cells, white blood cells, and platelets, resulting in anemia, leukopenia, and thrombocytopenia. Agranulocytosis specifically refers to an acute deficiency of granulocytes, particularly neutrophils, leading to increased vulnerability to infections. The key difference lies in pancytopenia affecting multiple blood cell types, whereas agranulocytosis predominantly involves granulocyte depletion.
Definition of Agranulocytosis
Agranulocytosis is a severe condition characterized by an extremely low count of granulocytes, particularly neutrophils, in the blood, leading to a heightened risk of infections. It is a subtype of pancytopenia, which denotes a reduction in all three blood cell types: red blood cells, white blood cells, and platelets. The critical difference lies in agranulocytosis specifically involving granulocyte depletion, whereas pancytopenia encompasses a broader deficiency in multiple blood cells.
Key Differences Between Pancytopenia and Agranulocytosis
Pancytopenia is characterized by a simultaneous reduction in red blood cells, white blood cells, and platelets, leading to anemia, increased infection risk, and bleeding tendencies, whereas agranulocytosis specifically refers to a severe decrease in neutrophils, a subset of white blood cells crucial for fighting bacterial infections. Pancytopenia results from bone marrow failure, aplasia, or infiltration, while agranulocytosis is often caused by drug reactions, autoimmune disorders, or infections targeting neutrophil production. Diagnostic differentiation relies on complete blood count analysis showing pancytopenia versus isolated neutropenia, guiding targeted treatment strategies and prognosis assessments.
Causes of Pancytopenia
Pancytopenia is commonly caused by bone marrow failure conditions such as aplastic anemia, myelodysplastic syndromes, and leukemia, as well as infections like HIV or tuberculosis and certain medications including chemotherapy agents and immunosuppressants. Nutritional deficiencies, particularly vitamin B12 or folate deficiency, also contribute significantly to pancytopenia. Agranulocytosis, in contrast, primarily results from drug-induced neutropenia, autoimmune diseases, or severe infections targeting granulocyte production.
Causes of Agranulocytosis
Agranulocytosis primarily results from drug-induced bone marrow suppression, with common causative agents including antithyroid medications, sulfonamides, and chemotherapy agents. Autoimmune disorders, viral infections like HIV or Epstein-Barr virus, and exposure to radiation can also trigger severe neutrophil depletion. Unlike pancytopenia, which involves a reduction in red blood cells, white blood cells, and platelets, agranulocytosis specifically denotes a critical drop in granulocytes, particularly neutrophils, increasing susceptibility to infections.
Clinical Presentation and Symptoms
Pancytopenia presents with generalized symptoms such as fatigue, pallor, increased susceptibility to infections, and bleeding tendencies due to the reduction of red blood cells, white blood cells, and platelets. Agranulocytosis primarily manifests with severe neutropenia symptoms, including sudden fever, chills, sore throat, and oral ulcers, reflecting an acute vulnerability to bacterial and fungal infections. Both conditions require prompt hematologic evaluation, but pancytopenia indicates a broader bone marrow impairment, whereas agranulocytosis specifically denotes critical neutrophil depletion.
Diagnostic Approaches and Laboratory Findings
Pancytopenia is characterized by a reduction in red blood cells, white blood cells, and platelets, typically diagnosed through a complete blood count (CBC) showing pancytopenia and confirmed by bone marrow biopsy revealing hypocellularity or infiltration. Agranulocytosis, marked by a severe decrease in neutrophils, is primarily diagnosed with a CBC indicating absolute neutrophil count below 500/mL, often confirmed with bone marrow examination showing granulocytic hypoplasia or aplasia. Laboratory findings distinguishing pancytopenia include pancytopenic indices across all cell lines, while agranulocytosis predominantly presents isolated neutropenia with preserved red blood cell and platelet counts.
Management and Treatment Options
Management of pancytopenia involves addressing the underlying cause, such as bone marrow suppression, with treatments including blood transfusions, immunosuppressive therapy, or hematopoietic stem cell transplantation. Agranulocytosis treatment requires prompt discontinuation of the offending drug, broad-spectrum antibiotics to prevent infection, and granulocyte colony-stimulating factor (G-CSF) to accelerate neutrophil recovery. Close monitoring of blood counts and supportive care are critical components in both conditions to reduce complications and improve patient outcomes.
Prognosis and Patient Outcomes
Pancytopenia, characterized by the reduction of red blood cells, white blood cells, and platelets, often has a variable prognosis depending on the underlying cause, such as bone marrow failure or malignancy, and may require treatments like bone marrow transplantation for improved patient outcomes. Agranulocytosis, marked by a severe decrease in neutrophils, poses a high risk of life-threatening infections, but with prompt identification and intervention, including discontinuation of causative drugs and administration of antibiotics or granulocyte colony-stimulating factor (G-CSF), patient outcomes can significantly improve. Prognosis in agranulocytosis is generally better when the condition is drug-induced and reversible, whereas pancytopenia outcomes depend more heavily on disease etiology and response to therapy.
Pancytopenia Infographic
 libterm.com
libterm.com