Hypoglycemia occurs when blood sugar levels drop below normal, causing symptoms like shakiness, sweating, confusion, and dizziness. Managing hypoglycemia involves rapid carbohydrate intake and understanding the underlying causes to prevent future episodes. Discover effective strategies to recognize, treat, and prevent hypoglycemia by reading the rest of the article.
Table of Comparison
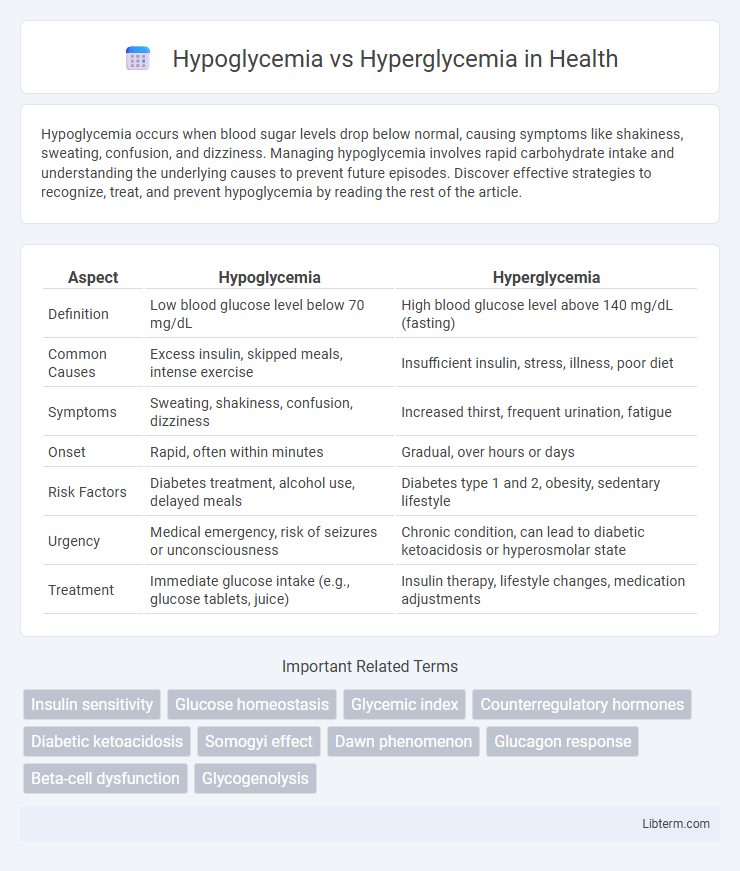
| Aspect | Hypoglycemia | Hyperglycemia |
|---|---|---|
| Definition | Low blood glucose level below 70 mg/dL | High blood glucose level above 140 mg/dL (fasting) |
| Common Causes | Excess insulin, skipped meals, intense exercise | Insufficient insulin, stress, illness, poor diet |
| Symptoms | Sweating, shakiness, confusion, dizziness | Increased thirst, frequent urination, fatigue |
| Onset | Rapid, often within minutes | Gradual, over hours or days |
| Risk Factors | Diabetes treatment, alcohol use, delayed meals | Diabetes type 1 and 2, obesity, sedentary lifestyle |
| Urgency | Medical emergency, risk of seizures or unconsciousness | Chronic condition, can lead to diabetic ketoacidosis or hyperosmolar state |
| Treatment | Immediate glucose intake (e.g., glucose tablets, juice) | Insulin therapy, lifestyle changes, medication adjustments |
Understanding Hypoglycemia and Hyperglycemia
Hypoglycemia occurs when blood glucose levels fall below 70 mg/dL, causing symptoms such as shakiness, confusion, and sweating, often requiring immediate intake of fast-acting carbohydrates. Hyperglycemia is characterized by blood glucose levels consistently above 130 mg/dL fasting or 180 mg/dL postprandial, leading to symptoms like increased thirst, frequent urination, and fatigue, and can result in long-term complications if unmanaged. Effective management of both conditions involves regular blood glucose monitoring, adherence to prescribed medication, and lifestyle adjustments to maintain glucose levels within target ranges.
Key Differences Between Hypoglycemia and Hyperglycemia
Hypoglycemia occurs when blood glucose levels drop below 70 mg/dL, causing symptoms like shakiness, sweating, and confusion, while hyperglycemia refers to blood glucose levels rising above 180 mg/dL, leading to increased thirst, frequent urination, and fatigue. Hypoglycemia requires immediate treatment with fast-acting carbohydrates to prevent severe complications such as seizures, whereas hyperglycemia management focuses on insulin therapy and monitoring to avoid long-term damage like neuropathy and cardiovascular disease. The underlying causes of hypoglycemia often include excessive insulin or medication, whereas hyperglycemia is primarily caused by insulin resistance or insufficient insulin production in diabetes.
Causes of Hypoglycemia
Hypoglycemia occurs when blood glucose levels drop below 70 mg/dL, primarily caused by excessive insulin administration, missed meals, intense physical activity, or certain medications like sulfonylureas. Other causes include alcohol consumption without food intake, hormone deficiencies (such as adrenal or pituitary insufficiency), and critical illnesses that impair glucose production. Understanding these factors is essential for managing and preventing hypoglycemic episodes in patients with diabetes and other metabolic disorders.
Causes of Hyperglycemia
Hyperglycemia occurs primarily due to insufficient insulin production or insulin resistance, often linked to type 1 and type 2 diabetes mellitus. Other causes include excessive carbohydrate intake, physical inactivity, stress, illness, and certain medications such as corticosteroids and thiazide diuretics. Chronic hyperglycemia can lead to serious complications like diabetic ketoacidosis, cardiovascular disease, and neuropathy.
Common Symptoms of Hypoglycemia
Hypoglycemia commonly presents with symptoms such as shakiness, sweating, confusion, and rapid heartbeat due to low blood glucose levels below 70 mg/dL. In contrast, hyperglycemia involves high blood sugar levels above 180 mg/dL, leading to symptoms like increased thirst, frequent urination, and fatigue. Recognizing hypoglycemia's early signs is critical to prevent severe complications such as seizures or loss of consciousness.
Common Symptoms of Hyperglycemia
Hyperglycemia commonly presents with increased thirst (polydipsia), frequent urination (polyuria), and blurred vision, often accompanied by fatigue and headache. Elevated blood glucose levels above 180 mg/dL cause osmotic diuresis, leading to dehydration and electrolyte imbalance. If untreated, hyperglycemia can progress to diabetic ketoacidosis, characterized by nausea, vomiting, and abdominal pain.
Diagnosis and Monitoring Techniques
Diagnosis of hypoglycemia involves measuring blood glucose levels below 70 mg/dL using point-of-care glucometers or continuous glucose monitors (CGMs) that provide real-time data. Hyperglycemia is diagnosed when fasting blood glucose exceeds 126 mg/dL or HbA1c levels are above 6.5%, assessed through laboratory blood tests or CGMs. Continuous monitoring with CGMs is critical for both conditions, allowing for timely detection of glucose fluctuations and improving management in diabetic patients.
Immediate Management Strategies
Hypoglycemia requires rapid administration of fast-acting carbohydrates such as glucose tablets or juice to quickly raise blood sugar levels, followed by a longer-acting carbohydrate to stabilize glucose. Hyperglycemia management focuses on insulin administration and hydration to reduce elevated blood glucose and prevent ketoacidosis. Continuous blood glucose monitoring and timely medical intervention are critical for both conditions to prevent severe complications.
Long-Term Prevention and Control
Effective long-term prevention and control of hypoglycemia and hyperglycemia rely on consistent blood glucose monitoring combined with personalized medication management. Lifestyle modifications such as balanced nutrition, regular physical activity, and stress management play a crucial role in maintaining optimal glycemic levels. Continuous patient education and regular healthcare consultations minimize complications like neuropathy, retinopathy, and cardiovascular disease associated with poorly controlled glucose levels.
When to Seek Medical Attention
Seek medical attention for hypoglycemia when blood glucose levels fall below 70 mg/dL accompanied by symptoms such as dizziness, confusion, sweating, or loss of consciousness. For hyperglycemia, immediate care is critical if blood sugar exceeds 300 mg/dL with signs like frequent urination, extreme thirst, nausea, or difficulty breathing, indicating possible diabetic ketoacidosis. Timely intervention prevents complications such as seizures, coma, and long-term organ damage.
Hypoglycemia Infographic
 libterm.com
libterm.com