Osteoarthritis is a common degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility. Effective management includes lifestyle changes, physical therapy, and medication to alleviate symptoms and improve joint function. Explore the rest of this article to learn how to protect your joints and maintain your quality of life.
Table of Comparison
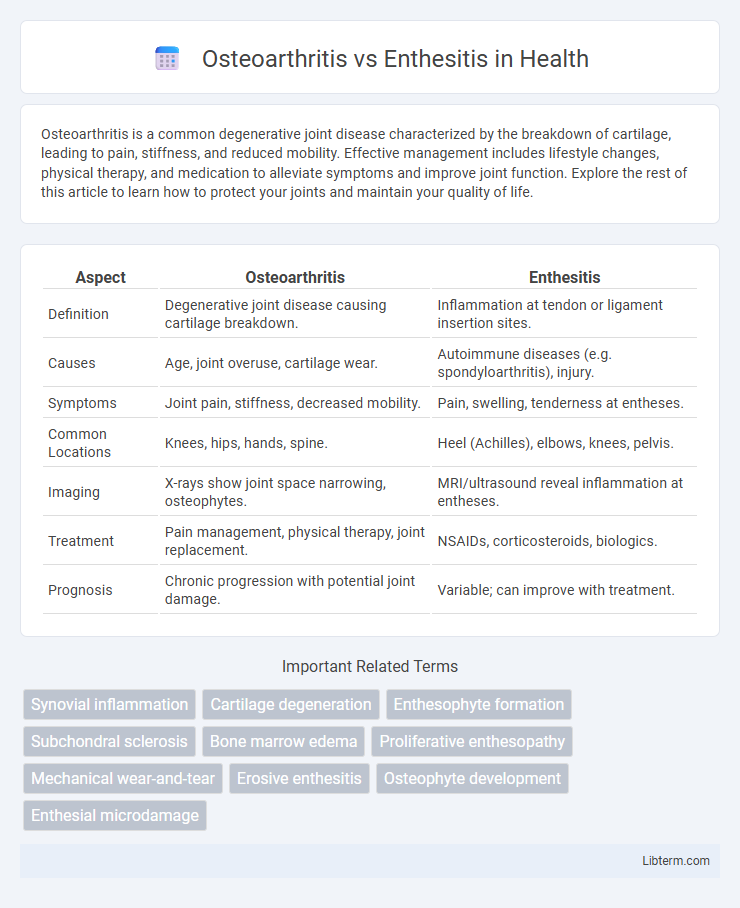
| Aspect | Osteoarthritis | Enthesitis |
|---|---|---|
| Definition | Degenerative joint disease causing cartilage breakdown. | Inflammation at tendon or ligament insertion sites. |
| Causes | Age, joint overuse, cartilage wear. | Autoimmune diseases (e.g. spondyloarthritis), injury. |
| Symptoms | Joint pain, stiffness, decreased mobility. | Pain, swelling, tenderness at entheses. |
| Common Locations | Knees, hips, hands, spine. | Heel (Achilles), elbows, knees, pelvis. |
| Imaging | X-rays show joint space narrowing, osteophytes. | MRI/ultrasound reveal inflammation at entheses. |
| Treatment | Pain management, physical therapy, joint replacement. | NSAIDs, corticosteroids, biologics. |
| Prognosis | Chronic progression with potential joint damage. | Variable; can improve with treatment. |
Understanding Osteoarthritis: Definition and Causes
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility, primarily affecting weight-bearing joints such as knees and hips. The condition results from wear and tear, age-related cartilage degradation, joint injuries, and genetic predisposition. Understanding the causes of osteoarthritis helps distinguish it from enthesitis, which involves inflammation at tendon or ligament attachment sites rather than cartilage deterioration.
What is Enthesitis? Key Characteristics
Enthesitis is the inflammation of entheses, the sites where tendons or ligaments attach to bone, commonly seen in spondyloarthropathies like psoriatic arthritis and ankylosing spondylitis. Key characteristics include localized pain, swelling, and tenderness at these attachment points, often affecting the Achilles tendon, plantar fascia, and costochondral joints. Unlike osteoarthritis, which involves cartilage degeneration and joint space narrowing, enthesitis primarily involves soft tissue inflammation without significant cartilage loss.
Differentiating Osteoarthritis and Enthesitis: Core Differences
Osteoarthritis primarily affects the cartilage and joints, leading to joint pain, stiffness, and reduced mobility due to cartilage degeneration and bone changes, commonly in weight-bearing joints like knees and hips. Enthesitis involves inflammation at the entheses, where tendons or ligaments attach to bone, causing localized pain and swelling, often associated with autoimmune conditions such as psoriatic arthritis or ankylosing spondylitis. Unlike the degenerative nature of osteoarthritis, enthesitis reflects an inflammatory process, with diagnostic imaging showing tendon or ligament inflammation rather than joint cartilage loss.
Common Symptoms: Osteoarthritis vs Enthesitis
Osteoarthritis commonly presents with joint pain, stiffness, and reduced range of motion, especially in weight-bearing joints like knees, hips, and hands, often worsening after activity. Enthesitis is characterized by inflammation at the sites where tendons or ligaments attach to bone, causing localized pain, tenderness, and swelling, frequently seen in conditions such as spondyloarthritis. While osteoarthritis symptoms are primarily mechanical and worsen with use, enthesitis involves inflammatory symptoms and may be accompanied by systemic signs like morning stiffness and fatigue.
Risk Factors: Who is Most Affected?
Osteoarthritis primarily affects older adults and is associated with risk factors such as age, obesity, joint injury, and repetitive joint stress. Enthesitis commonly occurs in younger individuals with spondyloarthritis and is linked to genetic predispositions like HLA-B27 positivity, as well as autoimmune conditions. Both conditions can be exacerbated by biomechanical stress, but their risk profiles differ significantly based on underlying causes and patient demographics.
Diagnosis: How Osteoarthritis and Enthesitis Are Identified
Osteoarthritis is primarily diagnosed through clinical evaluation, patient history, and imaging techniques such as X-rays and MRI, which reveal joint space narrowing, osteophyte formation, and cartilage degradation. Enthesitis diagnosis relies on physical examination showing tenderness at entheses sites and is confirmed with ultrasound or MRI, detecting inflammation, edema, and structural damage at tendon or ligament insertions. Laboratory tests are less definitive for osteoarthritis but may aid in ruling out inflammatory conditions linked to enthesitis, such as spondyloarthritis.
Treatment Options for Osteoarthritis
Osteoarthritis treatment primarily focuses on pain management and improving joint function through nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, and weight management. In advanced cases, corticosteroid injections or joint replacement surgery may be considered to alleviate symptoms and restore mobility. Unlike enthesitis, which often requires immunosuppressive therapies targeting inflammation, osteoarthritis treatment emphasizes mechanical support and symptomatic relief.
Management and Treatment of Enthesitis
Management of enthesitis primarily involves the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation at tendon or ligament insertion sites. Physical therapy and targeted exercises are critical to improve flexibility and strengthen the surrounding muscles, minimizing stress on affected entheses. In refractory cases, biologic agents such as tumor necrosis factor (TNF) inhibitors are effective in controlling persistent inflammation and preventing structural damage.
Prognosis and Long-Term Outcomes
Osteoarthritis often leads to progressive joint degeneration with variable pain management outcomes, frequently resulting in reduced mobility over time. Enthesitis, associated with inflammatory conditions like spondyloarthritis, may respond well to targeted anti-inflammatory treatments, potentially preventing severe structural damage if managed early. Long-term prognosis for enthesitis generally improves with proper immunomodulatory therapy, whereas osteoarthritis typically requires symptom management and lifestyle adaptations due to its chronic degenerative nature.
Prevention and Lifestyle Strategies
Osteoarthritis prevention centers on maintaining a healthy weight to reduce joint stress, engaging in low-impact exercises such as swimming or cycling to preserve joint mobility, and avoiding repetitive joint strain. Enthesitis management emphasizes early diagnosis, regular stretching, and strengthening exercises to reduce inflammation at tendon insertions, alongside maintaining a balanced diet rich in anti-inflammatory nutrients. Both conditions benefit from avoiding smoking and implementing ergonomic adjustments in daily activities to minimize joint and tendon irritation.
Osteoarthritis Infographic
 libterm.com
libterm.com