Hepatitis is an inflammation of the liver caused by viral infections, alcohol use, or autoimmune diseases, leading to symptoms such as jaundice, fatigue, and abdominal pain. Early diagnosis and treatment are critical to preventing severe liver damage and improving long-term health outcomes. Discover more about hepatitis types, risk factors, and effective treatment options in the rest of the article.
Table of Comparison
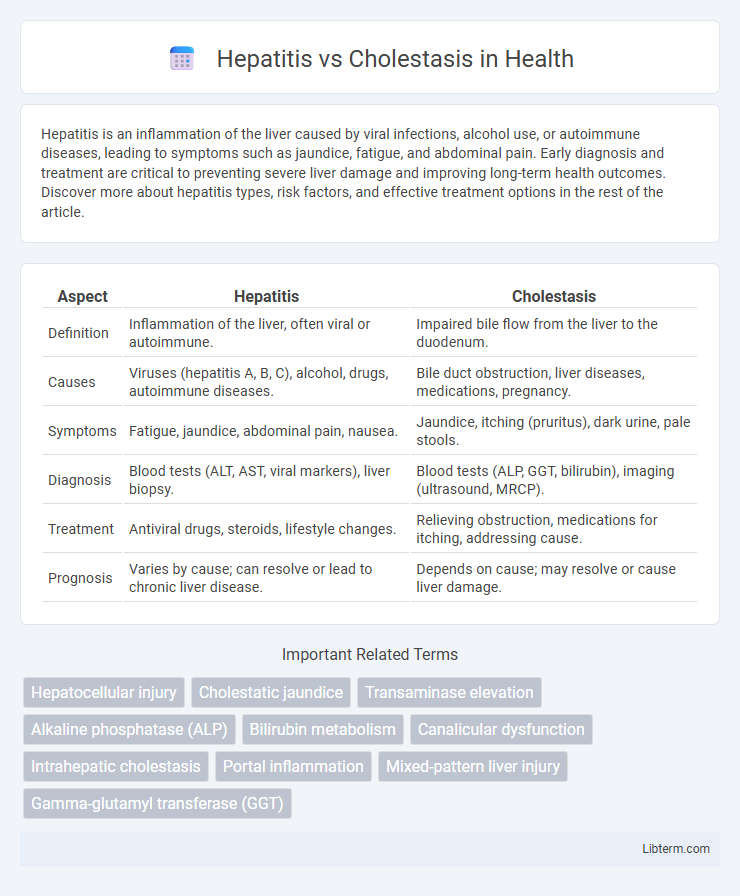
| Aspect | Hepatitis | Cholestasis |
|---|---|---|
| Definition | Inflammation of the liver, often viral or autoimmune. | Impaired bile flow from the liver to the duodenum. |
| Causes | Viruses (hepatitis A, B, C), alcohol, drugs, autoimmune diseases. | Bile duct obstruction, liver diseases, medications, pregnancy. |
| Symptoms | Fatigue, jaundice, abdominal pain, nausea. | Jaundice, itching (pruritus), dark urine, pale stools. |
| Diagnosis | Blood tests (ALT, AST, viral markers), liver biopsy. | Blood tests (ALP, GGT, bilirubin), imaging (ultrasound, MRCP). |
| Treatment | Antiviral drugs, steroids, lifestyle changes. | Relieving obstruction, medications for itching, addressing cause. |
| Prognosis | Varies by cause; can resolve or lead to chronic liver disease. | Depends on cause; may resolve or cause liver damage. |
Understanding Hepatitis and Cholestasis
Hepatitis is characterized by inflammation of the liver caused by viral infections, toxins, or autoimmune reactions, leading to symptoms such as jaundice, fatigue, and elevated liver enzymes. Cholestasis involves impaired bile flow from the liver to the duodenum, resulting in the accumulation of bile acids in the liver and bloodstream, which causes itching, jaundice, and dark urine. Differentiating hepatitis from cholestasis is critical for diagnosis and treatment, relying on liver function tests, imaging, and liver biopsy to assess inflammation, bile duct obstruction, and hepatocellular damage.
Key Differences Between Hepatitis and Cholestasis
Hepatitis primarily refers to inflammation of the liver caused by viral infections, toxins, or autoimmune conditions, leading to symptoms such as jaundice, fatigue, and elevated liver enzymes. Cholestasis involves impaired bile flow either due to intrahepatic damage or extrahepatic obstruction, resulting in bile accumulation, pruritus, and elevated serum bilirubin and alkaline phosphatase levels. The key difference lies in hepatitis as a direct inflammatory liver disease, while cholestasis is characterized by disrupted bile secretion and flow.
Causes of Hepatitis
Hepatitis is primarily caused by viral infections such as hepatitis A, B, C, D, and E, autoimmune diseases, excessive alcohol consumption, and exposure to toxic substances or certain medications. Cholestasis, by contrast, results from impaired bile flow due to bile duct obstruction, liver diseases, or genetic disorders. Understanding the causes of hepatitis is crucial for effective diagnosis and treatment, as it directly influences liver inflammation and damage.
Causes of Cholestasis
Cholestasis occurs due to impaired bile flow caused by factors such as bile duct obstruction, liver diseases like primary biliary cholangitis or primary sclerosing cholangitis, and drug-induced liver injury. In contrast, hepatitis primarily results from viral infections (hepatitis A, B, C), autoimmune disorders, or toxic injury affecting hepatocytes. Understanding cholestasis etiology involves identifying mechanical blockages, intrahepatic bile duct damage, and metabolic conditions disrupting bile secretion.
Clinical Symptoms Comparison
Hepatitis typically presents with clinical symptoms such as jaundice, fatigue, abdominal pain, and elevated liver enzymes, reflecting inflammation of liver tissue. Cholestasis primarily manifests through pruritus, dark urine, pale stools, and conjugated hyperbilirubinemia due to impaired bile flow. While both conditions cause jaundice, pruritus is more prominent in cholestasis, whereas systemic symptoms like malaise and anorexia are common in hepatitis.
Diagnostic Approaches
Diagnostic approaches for hepatitis primarily involve liver function tests (LFTs) showing elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, serologic markers for viral hepatitis, and liver biopsy for histological confirmation. In contrast, cholestasis diagnosis relies on elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) levels, imaging studies such as ultrasound, MRCP, or ERCP to identify bile duct obstruction, and bile acid analysis. Distinguishing features in diagnostics include the pattern of enzyme elevation and imaging findings that help differentiate hepatocellular injury in hepatitis from bile flow impairment in cholestasis.
Laboratory Findings: Hepatitis vs Cholestasis
Laboratory findings in hepatitis typically reveal elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, often exceeding 10 times the upper limit of normal, indicating hepatocellular injury. Cholestasis presents with significantly increased alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT), reflecting bile duct obstruction or impaired bile flow. Bilirubin elevation is common in both conditions but tends to be predominantly conjugated in cholestasis, whereas hepatitis can show mixed patterns depending on the extent of hepatocyte damage.
Treatment Strategies for Hepatitis and Cholestasis
Treatment strategies for hepatitis primarily focus on antiviral medications for viral hepatitis types B and C, immunosuppressive drugs for autoimmune hepatitis, and lifestyle modifications including abstaining from alcohol and maintaining a healthy diet to support liver function. Cholestasis management involves addressing the underlying cause such as bile duct obstruction or drug-induced cholestasis, utilizing bile acid sequestrants like ursodeoxycholic acid to improve bile flow, and symptom control for pruritus with antihistamines or rifampicin. Both conditions require careful monitoring of liver enzymes and function tests to evaluate treatment efficacy and prevent disease progression.
Prognosis and Complications
Hepatitis prognosis varies widely depending on the cause, with viral hepatitis often resolving with treatment, while chronic hepatitis can lead to cirrhosis and hepatocellular carcinoma. Cholestasis prognosis depends on the underlying etiology, where prolonged bile flow obstruction may result in biliary fibrosis, cirrhosis, and liver failure. Both conditions can cause complications such as jaundice, portal hypertension, and fat-soluble vitamin deficiencies, but hepatitis tends to have a higher risk of progression to liver cancer.
Prevention and Patient Management
Hepatitis prevention centers on vaccination for hepatitis A and B, safe needle practices, and avoiding contaminated food or water to reduce viral transmission. Cholestasis management involves identifying and treating underlying causes such as bile duct obstruction or drug-induced liver injury, with emphasis on symptom relief through bile acid sequestrants or ursodeoxycholic acid. Both conditions require regular liver function monitoring, lifestyle modifications including alcohol avoidance, and patient education to ensure early intervention and prevent progression to liver failure.
Hepatitis Infographic
 libterm.com
libterm.com