A hiatal hernia occurs when part of the stomach pushes up through the diaphragm into the chest cavity, often causing heartburn and acid reflux. Symptoms can vary from mild discomfort to severe pain, and lifestyle changes or medical treatments may be necessary to manage the condition effectively. Discover how understanding the causes and treatments of a hiatal hernia can improve your quality of life by reading the full article.
Table of Comparison
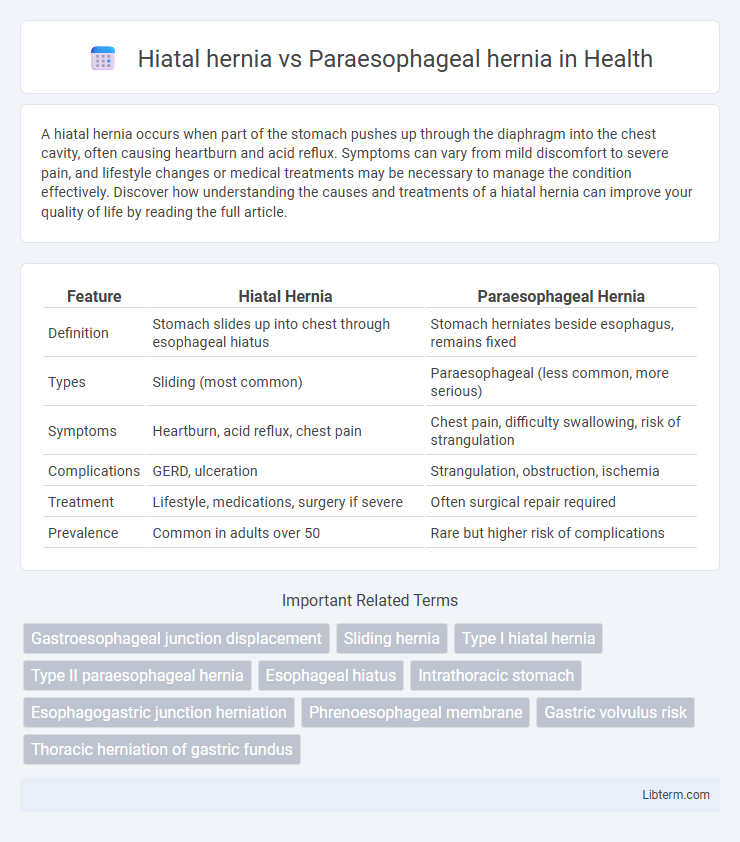
| Feature | Hiatal Hernia | Paraesophageal Hernia |
|---|---|---|
| Definition | Stomach slides up into chest through esophageal hiatus | Stomach herniates beside esophagus, remains fixed |
| Types | Sliding (most common) | Paraesophageal (less common, more serious) |
| Symptoms | Heartburn, acid reflux, chest pain | Chest pain, difficulty swallowing, risk of strangulation |
| Complications | GERD, ulceration | Strangulation, obstruction, ischemia |
| Treatment | Lifestyle, medications, surgery if severe | Often surgical repair required |
| Prevalence | Common in adults over 50 | Rare but higher risk of complications |
Introduction to Hiatal and Paraesophageal Hernias
Hiatal hernias occur when part of the stomach pushes through the diaphragm into the chest cavity, typically causing gastroesophageal reflux. Paraesophageal hernias are a less common but more serious type, where the stomach herniates beside the esophagus, risking strangulation and impaired blood flow. Understanding the anatomical differences and symptom presentations guides appropriate diagnosis and treatment strategies for these diaphragmatic hernias.
Anatomy of the Diaphragm and Esophageal Hiatus
The diaphragm's esophageal hiatus is a muscular opening allowing the esophagus to pass from the thorax to the abdomen, typically surrounded by the crura fibers. In a hiatal hernia, the stomach protrudes through this enlarged or weakened esophageal hiatus into the thoracic cavity, primarily involving the sliding of the gastroesophageal junction. Paraesophageal hernias occur when part of the stomach herniates adjacent to the esophagus through a defect in the diaphragm but the gastroesophageal junction remains in position, highlighting distinct anatomical disruptions at the esophageal hiatus.
What is a Hiatal Hernia?
A hiatal hernia occurs when the upper part of the stomach pushes through the diaphragm into the chest cavity, typically causing symptoms like acid reflux and heartburn. In contrast, a paraesophageal hernia involves the stomach herniating alongside the esophagus without the stomach sliding upward, posing a higher risk of complications such as strangulation. Understanding the structural differences between hiatal and paraesophageal hernias is crucial for accurate diagnosis and treatment planning.
What is a Paraesophageal Hernia?
A paraesophageal hernia occurs when part of the stomach pushes through the diaphragm beside the esophagus, unlike a hiatal hernia where the stomach slides upward through the hiatus. This type of hernia can cause serious complications such as stomach strangulation or obstruction due to the stomach's abnormal position. Diagnosis is often confirmed through imaging studies like barium swallow X-rays or endoscopy, which reveal the stomach's displacement adjacent to the esophagus.
Key Differences Between Hiatal and Paraesophageal Hernias
Hiatal hernia occurs when the stomach pushes through the diaphragm's esophageal hiatus into the chest cavity, primarily causing gastroesophageal reflux symptoms, while paraesophageal hernia involves part of the stomach herniating alongside the esophagus without reflux, posing risks of strangulation and obstruction. Hiatal hernias are often sliding types with intermittent symptoms, whereas paraesophageal hernias are fixed and may require surgical intervention due to higher complication risks. Diagnosis relies on imaging techniques like barium swallow X-rays and endoscopy to distinguish between the displacement of the gastroesophageal junction in hiatal hernias and the stomach's position adjacent to the esophagus in paraesophageal hernias.
Causes and Risk Factors
Hiatal hernias primarily result from weakness in the diaphragmatic muscle and increased intra-abdominal pressure, often influenced by obesity, aging, and heavy lifting. Paraesophageal hernias arise due to a defect or widening of the phrenoesophageal ligament, with risk factors including congenital abnormalities, trauma, and chronic straining. Both types are associated with conditions that increase pressure on the stomach, such as chronic coughing or pregnancy, but paraesophageal hernias pose a higher risk of complications like strangulation.
Signs and Symptoms Comparison
Hiatal hernia often presents with symptoms such as heartburn, acid reflux, and regurgitation due to the stomach sliding through the diaphragm into the chest cavity. Paraesophageal hernia, a less common but more serious condition, may cause chest pain, difficulty swallowing, and shortness of breath as the stomach herniates beside the esophagus, potentially leading to strangulation. While both hernias involve displacement of the stomach, signs of obstruction or ischemia are more prevalent in paraesophageal hernias, necessitating prompt medical evaluation.
Diagnostic Methods
Hiatal hernia diagnosis primarily relies on upper endoscopy, barium swallow radiography, and esophageal manometry to assess the hernia's size and its impact on the esophagus. Paraesophageal hernia detection frequently involves high-resolution computed tomography (CT) scans and endoscopic ultrasound to evaluate the herniated stomach portion and potential complications such as strangulation. Both conditions benefit from pH monitoring tests in cases where gastroesophageal reflux symptoms are present to determine esophageal acid exposure.
Treatment Options for Both Hernia Types
Treatment for hiatal hernia primarily involves lifestyle changes such as dietary adjustments, weight management, and medications like proton pump inhibitors to reduce acid reflux symptoms. Paraesophageal hernias often require surgical intervention, including laparoscopic hernia repair or fundoplication, due to risks of strangulation or obstruction. Both hernia types benefit from tailored approaches based on severity, symptomatology, and patient health status to optimize outcomes.
Prognosis and Complications
Hiatal hernia prognosis is generally favorable with lifestyle modifications and medication, though complications can include gastroesophageal reflux disease and esophagitis. Paraesophageal hernias pose a higher risk due to potential complications such as gastric volvulus, strangulation, and ischemia, which may require urgent surgical intervention. Long-term outcomes improve significantly following timely surgical repair, reducing risks of severe morbidity and mortality.
Hiatal hernia Infographic
 libterm.com
libterm.com