Lymphangitis is an inflammation of the lymphatic vessels typically caused by a bacterial infection, which can lead to red streaks on the skin, fever, and swollen lymph nodes. Early treatment with antibiotics is crucial to prevent the infection from spreading and causing serious complications. Learn more about the symptoms, causes, and effective treatments to protect your health in the rest of this article.
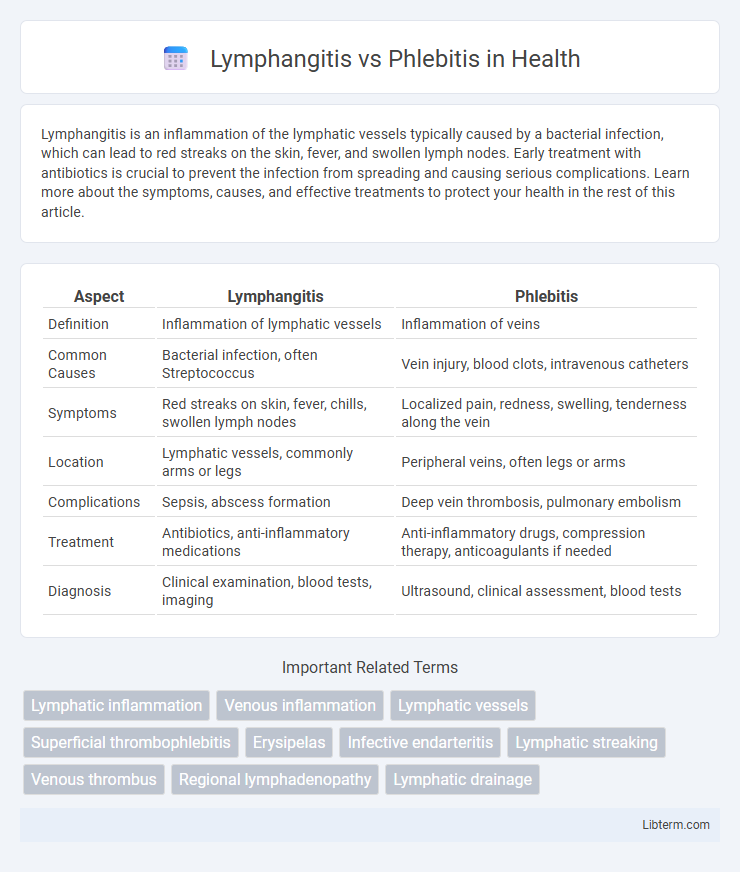
Table of Comparison
| Aspect | Lymphangitis | Phlebitis |
|---|---|---|
| Definition | Inflammation of lymphatic vessels | Inflammation of veins |
| Common Causes | Bacterial infection, often Streptococcus | Vein injury, blood clots, intravenous catheters |
| Symptoms | Red streaks on skin, fever, chills, swollen lymph nodes | Localized pain, redness, swelling, tenderness along the vein |
| Location | Lymphatic vessels, commonly arms or legs | Peripheral veins, often legs or arms |
| Complications | Sepsis, abscess formation | Deep vein thrombosis, pulmonary embolism |
| Treatment | Antibiotics, anti-inflammatory medications | Anti-inflammatory drugs, compression therapy, anticoagulants if needed |
| Diagnosis | Clinical examination, blood tests, imaging | Ultrasound, clinical assessment, blood tests |
Introduction to Lymphangitis and Phlebitis
Lymphangitis is an inflammation of the lymphatic vessels, often caused by bacterial infections such as Streptococcus pyogenes, leading to red streaks on the skin and swollen lymph nodes. Phlebitis refers to inflammation of a vein, commonly in the legs, typically associated with blood clots and characterized by pain, redness, and warmth along the affected vein. Both conditions involve inflammatory processes in vascular structures but differ in their anatomical targets and underlying causes.
Definition of Lymphangitis
Lymphangitis is an inflammation of the lymphatic vessels, often caused by a bacterial infection that spreads from a localized site into the lymphatic system. This condition typically presents with red streaks on the skin, fever, and tender lymph nodes, distinguishing it from phlebitis, which is inflammation of the veins. Understanding lymphangitis is crucial for early diagnosis and treatment to prevent systemic infection and complications.
Definition of Phlebitis
Phlebitis is defined as the inflammation of a vein, typically occurring in the superficial veins, often caused by trauma, infection, or intravenous catheter use. This condition results in pain, redness, and swelling along the affected vein, sometimes accompanied by thrombosis, known as superficial thrombophlebitis. Distinct from lymphangitis, which affects lymphatic vessels, phlebitis specifically involves venous inflammation and can lead to complications such as deep vein thrombosis if left untreated.
Causes of Lymphangitis vs Phlebitis
Lymphangitis is primarily caused by a bacterial infection, most commonly Streptococcus pyogenes, entering through a skin wound or ulcer, leading to inflammation of the lymphatic channels. Phlebitis results from vein inflammation often triggered by intravenous catheter use, varicose veins, or blood clot formation, with causes including trauma, infection, or chronic venous insufficiency. Understanding the distinct etiologies--bacterial invasion for lymphangitis and mechanical or thrombotic factors for phlebitis--is crucial for accurate diagnosis and treatment.
Key Symptoms and Clinical Presentation
Lymphangitis presents with red streaks extending from the site of infection, fever, chills, and swollen, tender lymph nodes, often indicating an underlying bacterial infection spreading through lymphatic vessels. Phlebitis is characterized by localized pain, redness, warmth, and swelling along a superficial vein, sometimes with palpable cord-like veins, typically caused by inflammation or thrombosis. Both conditions require clinical evaluation, but lymphangitis frequently signifies systemic involvement, whereas phlebitis is usually more localized.
Diagnostic Differences
Lymphangitis diagnosis primarily involves identifying red streaks along lymphatic vessels, often confirmed through clinical examination and patient history of infection. In contrast, phlebitis diagnosis relies on detecting inflammation of superficial veins through ultrasound imaging and assessing symptoms such as localized pain, swelling, and palpable cord-like veins. Laboratory tests including blood cultures and inflammatory markers help differentiate lymphangitis caused by bacterial infections from phlebitis, which may be associated with thrombosis or intravenous catheter use.
Risk Factors and Predisposing Conditions
Lymphangitis primarily arises from bacterial infections, with risk factors including skin wounds, insect bites, and compromised immune systems, especially in diabetic or immunosuppressed patients. Phlebitis is often linked to intravenous catheter use, varicose veins, and thrombophlebitis, with predisposing conditions such as venous stasis, obesity, and a history of deep vein thrombosis (DVT). Both conditions share common risk elements like poor hygiene and systemic infections but differ in their vascular involvement and typical causative agents.
Treatment and Management Approaches
Treatment of lymphangitis primarily involves high-dose intravenous antibiotics targeting common causative bacteria such as Streptococcus pyogenes and Staphylococcus aureus to prevent systemic infection. Phlebitis management emphasizes both pharmacological intervention with nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and mechanical methods such as compression therapy to promote venous flow and prevent thrombus progression. In both conditions, early diagnosis and appropriate wound care are critical to avoid complications, with surgical intervention reserved for abscess drainage or severe cases.
Complications and Prognosis
Lymphangitis complications include sepsis, abscess formation, and chronic lymphedema, often requiring prompt antibiotic treatment to prevent systemic spread. Phlebitis complications involve deep vein thrombosis (DVT), pulmonary embolism, and post-thrombotic syndrome, which can lead to long-term venous insufficiency. Prognosis for lymphangitis improves significantly with early intervention, while phlebitis prognosis depends on the extent of thrombosis and timely anticoagulant therapy.
Prevention Strategies and Patient Education
Effective prevention of lymphangitis and phlebitis involves maintaining proper skin hygiene to reduce infection risk and managing underlying venous conditions through regular exercise and compression therapy. Patient education should emphasize early recognition of symptoms such as redness, swelling, and pain, encouraging prompt medical evaluation to prevent complications. Avoiding prolonged immobility and careful care of intravenous sites further reduces incidence and supports vascular health.
Lymphangitis Infographic
 libterm.com
libterm.com