Hepatomegaly refers to the abnormal enlargement of the liver, which can result from various underlying conditions such as infections, liver diseases, or congestive heart failure. Recognizing the symptoms and causes of hepatomegaly is crucial for accurate diagnosis and effective treatment. Delve into this article to understand more about hepatomegaly and how it may affect your health.
Table of Comparison
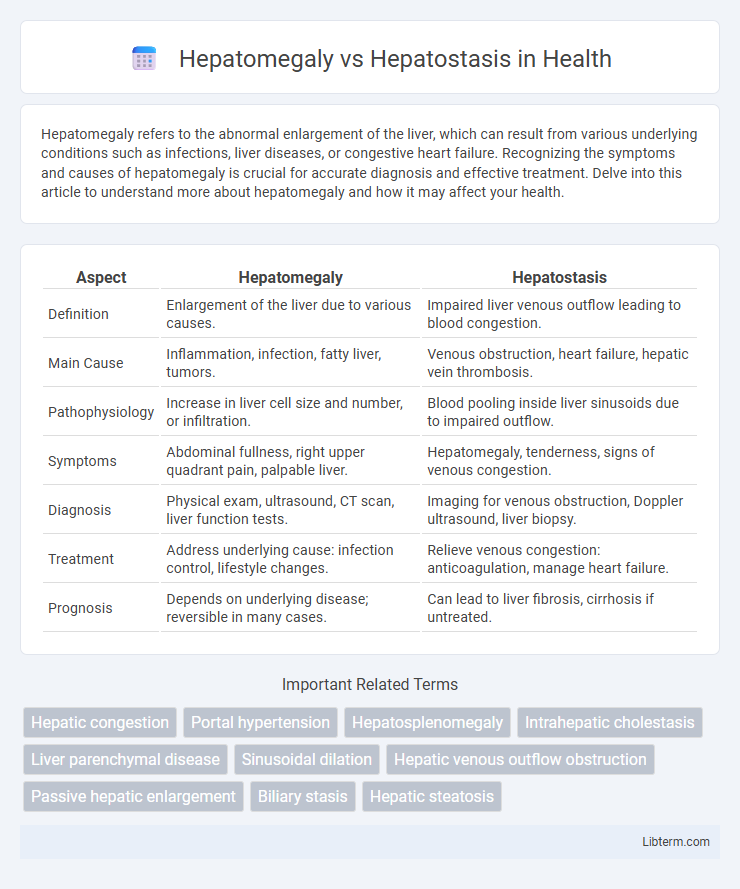
| Aspect | Hepatomegaly | Hepatostasis |
|---|---|---|
| Definition | Enlargement of the liver due to various causes. | Impaired liver venous outflow leading to blood congestion. |
| Main Cause | Inflammation, infection, fatty liver, tumors. | Venous obstruction, heart failure, hepatic vein thrombosis. |
| Pathophysiology | Increase in liver cell size and number, or infiltration. | Blood pooling inside liver sinusoids due to impaired outflow. |
| Symptoms | Abdominal fullness, right upper quadrant pain, palpable liver. | Hepatomegaly, tenderness, signs of venous congestion. |
| Diagnosis | Physical exam, ultrasound, CT scan, liver function tests. | Imaging for venous obstruction, Doppler ultrasound, liver biopsy. |
| Treatment | Address underlying cause: infection control, lifestyle changes. | Relieve venous congestion: anticoagulation, manage heart failure. |
| Prognosis | Depends on underlying disease; reversible in many cases. | Can lead to liver fibrosis, cirrhosis if untreated. |
Introduction to Hepatomegaly and Hepatostasis
Hepatomegaly refers to the abnormal enlargement of the liver, often caused by conditions such as fatty liver disease, hepatitis, or congestive heart failure. Hepatostasis, on the other hand, is characterized by impaired liver function due to congestion or blood flow obstruction, commonly seen in right-sided heart failure. Understanding the distinction between hepatomegaly and hepatostasis is essential for accurate diagnosis and targeted treatment of liver-related disorders.
Defining Hepatomegaly: Causes and Clinical Significance
Hepatomegaly refers to the abnormal enlargement of the liver, often caused by conditions such as hepatic congestion, fatty liver disease, hepatitis, or malignancies, indicating underlying pathology. This enlargement can signal hepatic dysfunction, systemic diseases like heart failure, or infiltrative disorders, making it an important diagnostic clue. Differentiating hepatomegaly from hepatostasis--the stagnation of blood flow within the liver--is critical, as hepatostasis primarily reflects impaired hepatic circulation rather than structural liver enlargement.
Understanding Hepatostasis: Pathophysiology and Etiology
Hepatostasis refers to impaired liver blood flow resulting from venous outflow obstruction, leading to hepatic congestion and hypoxia without primary liver cell damage. Its pathophysiology involves conditions such as Budd-Chiari syndrome, right-sided heart failure, or constrictive pericarditis, which increase hepatic venous pressure and disrupt normal hepatic microcirculation. Unlike hepatomegaly, which denotes an enlarged liver due to various causes, hepatostasis specifically highlights the circulatory impairment underlying liver dysfunction.
Key Differences Between Hepatomegaly and Hepatostasis
Hepatomegaly refers to the abnormal enlargement of the liver, often caused by conditions such as hepatitis, fatty liver disease, or congestive heart failure, whereas hepatostasis involves impaired bile flow leading to cholestasis without significant liver enlargement. Hepatomegaly is typically detected through physical examination or imaging studies showing increased liver size, while hepatostasis is diagnosed via biochemical markers like elevated bilirubin and alkaline phosphatase levels indicating bile retention. The primary difference lies in hepatomegaly representing structural liver enlargement, whereas hepatostasis indicates functional biliary obstruction or impaired bile secretion.
Common Signs and Symptoms: Hepatomegaly vs Hepatostasis
Hepatomegaly is characterized by an enlarged liver often palpable below the right costal margin, accompanied by symptoms such as abdominal fullness, discomfort, and sometimes jaundice. Hepatostasis, or liver congestion, typically presents with a normal-sized or slightly enlarged liver and signs like dull right upper quadrant pain, hepatomegaly in severe cases, and symptoms of underlying heart failure or venous obstruction. Both conditions may show elevated liver enzymes, but hepatomegaly frequently results from direct liver pathology, whereas hepatostasis is primarily due to impaired hepatic venous outflow.
Diagnostic Approaches for Hepatic Enlargement and Stasis
Diagnostic approaches for hepatic enlargement, or hepatomegaly, primarily include abdominal ultrasound, which assesses liver size and echotexture, while CT scans and MRI provide detailed anatomical information and help identify underlying causes such as tumors or fatty infiltration. Hepatostasis, characterized by impaired bile flow and liver congestion, is commonly evaluated through liver function tests, cholangiography, and Doppler ultrasound to detect vascular abnormalities or bile duct obstructions. Biopsy and elastography are additional tools used in complex cases to differentiate between structural enlargement in hepatomegaly and functional stasis impacting hepatic tissue.
Imaging Techniques in Differentiating Liver Disorders
Imaging techniques such as ultrasound, CT scan, and MRI are essential for differentiating hepatomegaly from hepatostasis by assessing liver size, texture, and blood flow. Ultrasound provides real-time evaluation of liver enlargement and vascular congestion, while CT and MRI offer detailed anatomical and functional information highlighting structural abnormalities or venous outflow obstruction. Doppler ultrasound enhances detection of hepatostasis by visualizing impaired hepatic vein flow, facilitating accurate diagnosis and targeted treatment planning.
Treatment Strategies for Hepatomegaly and Hepatostasis
Treatment strategies for hepatomegaly focus on addressing the underlying cause, such as infections, metabolic disorders, or congestive heart failure, often involving antiviral medications, lifestyle modifications, or diuretics. Hepatostasis treatment aims to improve hepatic blood flow and reduce congestion, commonly managed through vasodilators, anticoagulants, and managing right-sided heart failure. Both conditions may require supportive care including dietary adjustments and monitoring liver function to prevent progression and complications.
Potential Complications and Prognosis
Hepatomegaly, characterized by an enlarged liver, can lead to complications such as liver dysfunction, portal hypertension, and increased risk of cirrhosis or liver failure. Hepatostasis, indicating impaired liver blood flow without significant enlargement, primarily risks hepatic ischemia, congestion, and subsequent necrosis, potentially progressing to acute liver injury. Prognosis in hepatomegaly depends on the underlying cause and extent of liver damage, whereas hepatostasis prognosis varies with timely restoration of hepatic circulation and prevention of ischemic injury.
Summary: Choosing the Right Management Path
Hepatomegaly involves pathological liver enlargement due to conditions like infections, fatty liver, or malignancies, requiring targeted treatment to address the underlying cause. Hepatostasis, characterized by impaired bile flow and liver congestion, demands management focused on relieving biliary obstruction and improving hepatic drainage. Accurate diagnosis differentiating these conditions guides effective therapeutic strategies, optimizing patient outcomes through tailored interventions such as pharmacotherapy for hepatomegaly or surgical procedures for hepatostasis.
Hepatomegaly Infographic
 libterm.com
libterm.com