Onychomycosis and eczema can both affect your nails, causing discoloration, thickening, and discomfort, but they have different underlying causes and treatments. Proper diagnosis is essential to differentiate between the fungal infection of onychomycosis and the inflammatory nature of eczema to ensure effective management. Explore the rest of the article to understand the symptoms, diagnosis, and treatment options for these nail conditions.
Table of Comparison
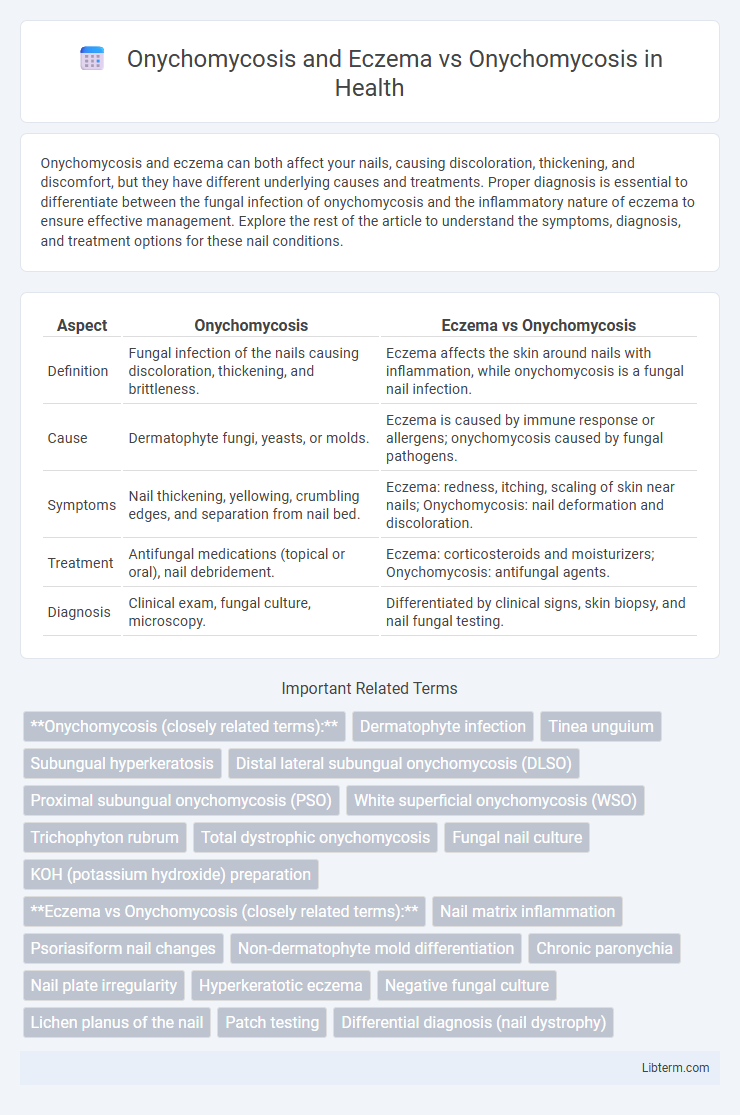
| Aspect | Onychomycosis | Eczema vs Onychomycosis |
|---|---|---|
| Definition | Fungal infection of the nails causing discoloration, thickening, and brittleness. | Eczema affects the skin around nails with inflammation, while onychomycosis is a fungal nail infection. |
| Cause | Dermatophyte fungi, yeasts, or molds. | Eczema is caused by immune response or allergens; onychomycosis caused by fungal pathogens. |
| Symptoms | Nail thickening, yellowing, crumbling edges, and separation from nail bed. | Eczema: redness, itching, scaling of skin near nails; Onychomycosis: nail deformation and discoloration. |
| Treatment | Antifungal medications (topical or oral), nail debridement. | Eczema: corticosteroids and moisturizers; Onychomycosis: antifungal agents. |
| Diagnosis | Clinical exam, fungal culture, microscopy. | Differentiated by clinical signs, skin biopsy, and nail fungal testing. |
Understanding Onychomycosis: Causes and Symptoms
Onychomycosis, primarily caused by dermatophyte fungi such as Trichophyton rubrum, results in nail discoloration, thickening, and crumbling, distinguishing it from eczema which primarily affects the skin with inflammation and itching. Symptoms of onychomycosis include yellow or white nail spots, brittle nails, and sometimes pain, whereas eczema-related nail changes often involve ridging, pitting, and periungual dermatitis. Accurate diagnosis requires recognizing fungal infection indicators like subungual debris, contrasting with eczema's skin-based symptoms, to guide effective treatment strategies.
What Is Eczema? Key Features and Triggers
Eczema, also known as atopic dermatitis, is a chronic inflammatory skin condition characterized by red, itchy, and dry patches, often accompanied by swelling and blistering, differing from onychomycosis, which is a fungal infection of the nails. Key triggers for eczema include allergens like pollen, dust mites, irritants such as soaps and detergents, extreme temperatures, and stress, which cause immune system reactions leading to skin inflammation. Unlike onychomycosis that primarily affects nail structure and color, eczema impacts the skin barrier function, resulting in increased sensitivity and vulnerability to infections.
Differentiating Onychomycosis from Eczema
Differentiating onychomycosis from eczema involves evaluating key clinical and diagnostic features; onychomycosis typically presents with thickened, discolored, and brittle nails caused by fungal infection, while eczema-related nail changes often include pitting, ridging, and periungual inflammation associated with dermatitis. Microscopic examination and fungal cultures confirm onychomycosis, distinguishing it from eczema, which lacks fungal involvement and responds to anti-inflammatory treatments. Accurate diagnosis is crucial for optimal management, as onychomycosis requires antifungal therapy whereas eczema improves with topical corticosteroids and moisturizers.
Common Misdiagnoses: Eczema vs. Fungal Nail Infections
Onychomycosis, a fungal nail infection, is frequently misdiagnosed as eczema due to overlapping symptoms such as nail discoloration, thickening, and inflammation. Dermatologists emphasize accurate diagnosis through mycological examination and culture to distinguish between eczema-related nail changes and fungal infections, as treatment approaches differ significantly. Misdiagnosis can lead to ineffective therapy, prolonged discomfort, and potential worsening of the condition, highlighting the need for precise clinical and laboratory assessment.
Clinical Signs: Onychomycosis Compared to Eczema
Onychomycosis presents with clinical signs such as thickened, discolored, brittle nails, often accompanied by subungual debris and nail plate distortion. In contrast, eczema affecting the nails typically shows periungual inflammation, erythema, scaling, and sometimes nail pitting or ridging without the fungal invasion seen in onychomycosis. Differentiating these conditions relies on recognizing fungal involvement in onychomycosis versus inflammatory changes in eczema.
Diagnostic Techniques for Nail Disorders
Differentiating Onychomycosis from Eczema requires precise diagnostic techniques such as direct microscopy, fungal culture, and PCR analysis to detect fungal pathogens, while eczema diagnosis relies more on clinical evaluation and skin biopsy. Dermoscopy can aid in identifying characteristic nail changes, with Onychomycosis showing longitudinal streaks and subungual debris, contrasting with the inflammatory signs typical of Eczema. Accurate diagnosis ensures targeted treatment, reducing misdiagnosis and improving patient outcomes in nail disorders.
Treatment Approaches: Onychomycosis vs. Eczema Management
Treatment approaches for onychomycosis primarily involve antifungal medications such as terbinafine or itraconazole, often administered orally or topically, targeting fungal pathogens directly. Eczema management focuses on reducing inflammation and itchiness with corticosteroids, moisturizers, and avoiding irritants, without antifungal agents. Accurate diagnosis is crucial as misidentifying onychomycosis for eczema can delay appropriate antifungal treatment and worsen the fungal infection.
Preventive Strategies for Nail Health
Effective preventive strategies for Onychomycosis and Eczema focus on maintaining nail hygiene, avoiding prolonged moisture exposure, and using antifungal or moisturizing treatments to reduce fungal growth and skin irritation. Differentiating between these conditions is crucial, as Eczema requires emollients to restore the skin barrier, while Onychomycosis necessitates antifungal agents to eliminate infection. Regular nail care, including trimming, avoiding trauma, and using breathable footwear, helps prevent both fungal infections and eczema-related complications, promoting overall nail health.
When to See a Dermatologist: Warning Signs
Persistent nail discoloration, thickening, or crumbling may indicate onychomycosis and warrant a dermatologist's evaluation, especially if accompanied by painful or spreading skin lesions typical of eczema. Immediate medical attention is necessary when nails exhibit sudden changes, such as swelling, redness, or oozing, which may signal secondary infections or complications. Early diagnosis by a dermatologist ensures accurate differentiation between onychomycosis and eczema, facilitating targeted treatment and preventing chronic nail damage.
FAQs: Managing Onychomycosis and Eczema Affecting Nails
Managing onychomycosis and eczema affecting nails involves distinguishing fungal infections from inflammatory skin conditions to ensure accurate treatment. Antifungal medications effectively target onychomycosis, while eczema management requires topical corticosteroids and moisturizers to reduce inflammation and prevent flare-ups. Regular nail hygiene, avoiding irritants, and consulting a dermatologist for biopsy or culture tests are essential for diagnosis and tailored therapy.
Onychomycosis and Eczema Infographic
 libterm.com
libterm.com