Gynecomastia and lipomastia are common conditions involving abnormal breast tissue enlargement in males, with gynecomastia characterized by glandular tissue growth and lipomastia caused by excess fat accumulation. Understanding the differences between these conditions is crucial for accurate diagnosis and appropriate treatment, as they require distinct medical approaches. Explore the rest of the article to learn how you can identify symptoms and find effective solutions for each condition.
Table of Comparison
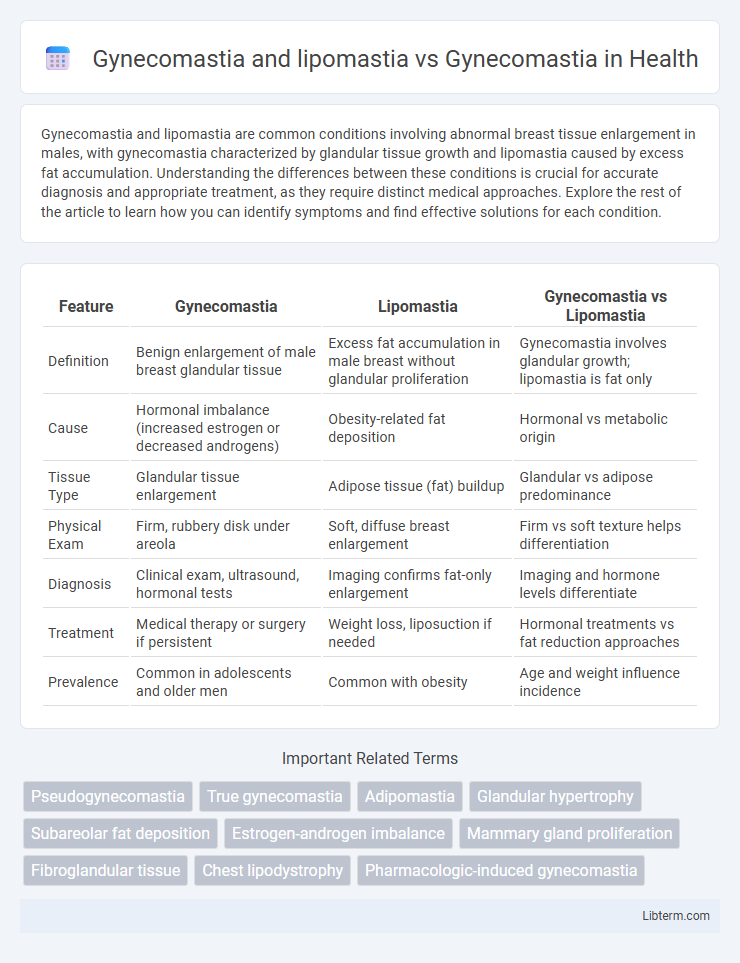
| Feature | Gynecomastia | Lipomastia | Gynecomastia vs Lipomastia |
|---|---|---|---|
| Definition | Benign enlargement of male breast glandular tissue | Excess fat accumulation in male breast without glandular proliferation | Gynecomastia involves glandular growth; lipomastia is fat only |
| Cause | Hormonal imbalance (increased estrogen or decreased androgens) | Obesity-related fat deposition | Hormonal vs metabolic origin |
| Tissue Type | Glandular tissue enlargement | Adipose tissue (fat) buildup | Glandular vs adipose predominance |
| Physical Exam | Firm, rubbery disk under areola | Soft, diffuse breast enlargement | Firm vs soft texture helps differentiation |
| Diagnosis | Clinical exam, ultrasound, hormonal tests | Imaging confirms fat-only enlargement | Imaging and hormone levels differentiate |
| Treatment | Medical therapy or surgery if persistent | Weight loss, liposuction if needed | Hormonal treatments vs fat reduction approaches |
| Prevalence | Common in adolescents and older men | Common with obesity | Age and weight influence incidence |
Introduction to Male Breast Enlargement
Male breast enlargement includes gynecomastia, characterized by glandular tissue proliferation, and lipomastia, defined by excess fatty tissue without glandular growth; distinguishing these conditions is crucial for accurate diagnosis and treatment. Gynecomastia results from hormonal imbalances, often due to increased estrogen or decreased androgen activity, while lipomastia is primarily linked to obesity and adipose tissue accumulation. Understanding these differences enables targeted medical or surgical interventions, improving patient outcomes in managing male breast enlargement.
Understanding Gynecomastia
Gynecomastia is characterized by the benign enlargement of male breast glandular tissue, distinct from lipomastia, which involves excess fat accumulation without glandular growth. Understanding gynecomastia requires recognizing its hormonal imbalances, often due to increased estrogen or decreased testosterone levels, leading to true breast tissue proliferation. Accurate diagnosis differentiates gynecomastia from lipomastia, guiding targeted treatment approaches such as hormone therapy or surgical intervention.
What is Lipomastia (Pseudogynecomastia)?
Lipomastia, or pseudogynecomastia, is the accumulation of excess fatty tissue in the male breast area without the presence of glandular breast tissue, distinguishing it from true gynecomastia, which involves glandular proliferation. Unlike gynecomastia, which results from hormonal imbalances leading to breast tissue growth, pseudogynecomastia is primarily caused by increased adipose tissue often linked to obesity or weight gain. Understanding this difference is crucial for determining appropriate treatment, with lipomastia typically managed through weight loss or liposuction rather than hormone therapy or glandular tissue excision.
Key Differences: Gynecomastia vs. Lipomastia
Gynecomastia involves the benign enlargement of male breast glandular tissue, often caused by hormonal imbalances, while lipomastia is characterized by excess fatty tissue without glandular proliferation. Unlike gynecomastia, lipomastia typically results from weight gain and obesity, lacking the distinct firm glandular mass felt in true gynecomastia. Diagnosis relies on clinical examination and imaging to differentiate glandular hypertrophy from adipose accumulation, guiding appropriate treatment options.
Symptoms and Physical Characteristics
Gynecomastia presents as a firm, rubbery mass of glandular breast tissue beneath the nipple, often accompanied by tenderness or pain, whereas lipomastia involves fatty tissue enlargement without a distinct glandular mass. Symptoms of gynecomastia include swelling and sensitivity around the nipple-areolar complex, while lipomastia typically lacks tenderness and presents as soft, diffuse breast enlargement. Differentiating these conditions is crucial for diagnosis, as gynecomastia indicates glandular proliferation, and lipomastia results primarily from adipose tissue accumulation.
Causes and Risk Factors
Gynecomastia is primarily caused by hormonal imbalances, particularly an increase in estrogen or a decrease in testosterone, which can result from puberty, aging, certain medications, or underlying health conditions such as liver or kidney disease. Lipomastia, often mistaken for gynecomastia, involves the accumulation of fatty tissue without glandular proliferation, commonly associated with obesity and metabolic disorders. Risk factors for gynecomastia include the use of anabolic steroids, alcohol abuse, and endocrine disorders, whereas lipomastia is predominantly linked to excess weight and poor diet.
Diagnostic Methods
Gynecomastia and lipomastia differ significantly in diagnostic approaches, with gynecomastia involving the proliferation of glandular breast tissue and lipomastia characterized by excess fatty tissue. Diagnostic methods for gynecomastia include physical examination, ultrasound imaging to differentiate between fatty and glandular tissue, and hormonal assays to identify underlying endocrine causes. Lipomastia diagnosis relies primarily on clinical assessment and imaging techniques such as mammography or MRI to exclude true glandular enlargement typical of gynecomastia.
Treatment Options for Gynecomastia
Treatment options for gynecomastia include surgical interventions such as liposuction and mastectomy to remove excess glandular tissue and fat, particularly distinguishing cases of gynecomastia from lipomastia where fat accumulation predominates. Non-surgical treatments involve hormone therapy using selective estrogen receptor modulators (SERMs) like tamoxifen to address hormonal imbalances contributing to glandular enlargement. Postoperative care and lifestyle modifications play a crucial role in preventing recurrence and enhancing aesthetic outcomes in patients diagnosed with true gynecomastia.
Management Strategies for Lipomastia
Management strategies for lipomastia primarily involve targeted liposuction or ultrasound-assisted liposuction to remove excess fat deposits in the male breast, distinguishing it from gynecomastia treatment, which often requires surgical excision of glandular tissue. Accurate diagnosis using ultrasound or mammography is crucial to differentiate lipomastia from true gynecomastia and guide appropriate intervention. Lifestyle modifications, such as weight loss through diet and exercise, can complement surgical management by addressing underlying adipose tissue accumulation.
Prevention and Lifestyle Recommendations
Maintaining a balanced diet low in processed foods and rich in antioxidants helps reduce the risk of both gynecomastia and lipomastia by managing body fat and hormonal levels. Regular cardiovascular exercise and strength training promote healthy weight and muscle mass, which are crucial in preventing excess fat deposition characteristic of lipomastia and hormonal imbalances linked to gynecomastia. Avoiding substances such as anabolic steroids, alcohol, and certain medications can also mitigate gynecomastia symptoms by supporting normal endocrine function.
Gynecomastia and lipomastia Infographic
 libterm.com
libterm.com