Hyperparathyroidism is a condition characterized by the overproduction of parathyroid hormone, leading to elevated calcium levels in the blood and potential complications such as kidney stones, osteoporosis, and fatigue. Early diagnosis and effective management are crucial to prevent severe health issues and improve your quality of life. Explore the entire article to understand symptoms, causes, and treatment options for hyperparathyroidism.
Table of Comparison
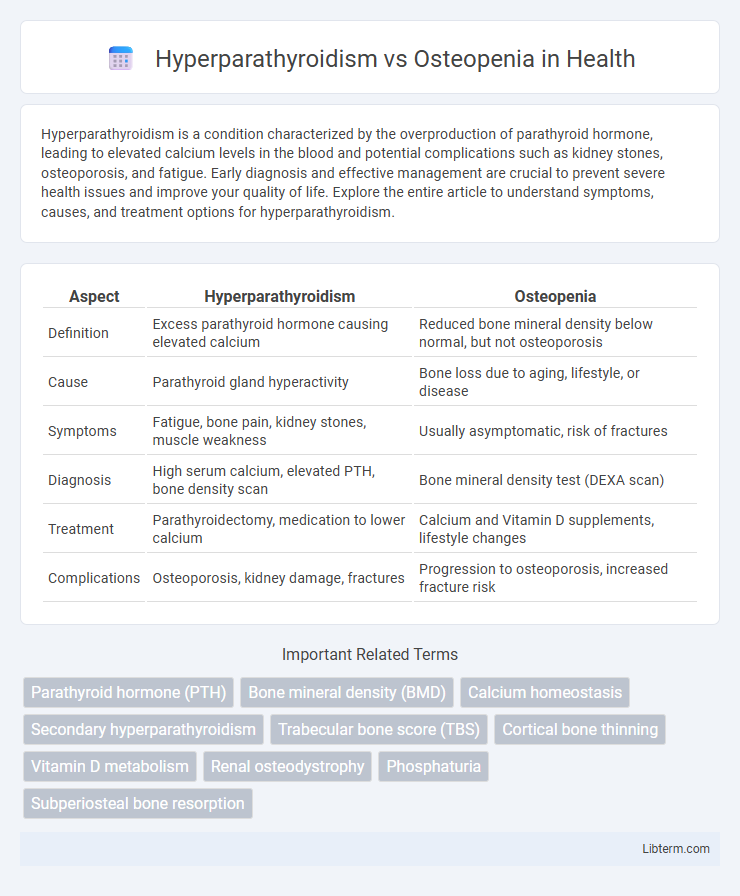
| Aspect | Hyperparathyroidism | Osteopenia |
|---|---|---|
| Definition | Excess parathyroid hormone causing elevated calcium | Reduced bone mineral density below normal, but not osteoporosis |
| Cause | Parathyroid gland hyperactivity | Bone loss due to aging, lifestyle, or disease |
| Symptoms | Fatigue, bone pain, kidney stones, muscle weakness | Usually asymptomatic, risk of fractures |
| Diagnosis | High serum calcium, elevated PTH, bone density scan | Bone mineral density test (DEXA scan) |
| Treatment | Parathyroidectomy, medication to lower calcium | Calcium and Vitamin D supplements, lifestyle changes |
| Complications | Osteoporosis, kidney damage, fractures | Progression to osteoporosis, increased fracture risk |
Introduction to Hyperparathyroidism and Osteopenia
Hyperparathyroidism is a condition characterized by excessive secretion of parathyroid hormone (PTH), leading to elevated calcium levels and potential bone resorption. Osteopenia is a bone disorder marked by lower than normal bone mineral density, serving as a precursor to osteoporosis. Both conditions impact bone health but differ in their underlying causes and biochemical markers.
Understanding Hyperparathyroidism: Causes and Symptoms
Hyperparathyroidism is a condition characterized by excessive secretion of parathyroid hormone (PTH), primarily caused by parathyroid adenomas, hyperplasia, or, rarely, carcinoma. Elevated PTH levels lead to increased calcium resorption from bones, resulting in weakened bone density and symptoms such as bone pain, fractures, kidney stones, fatigue, and abdominal discomfort. Distinguishing hyperparathyroidism from osteopenia is essential, as osteopenia involves reduced bone mineral density without the endocrine imbalance or systemic symptoms seen in hyperparathyroidism.
Defining Osteopenia: Risk Factors and Manifestations
Osteopenia is characterized by decreased bone mineral density, serving as a precursor to osteoporosis and increasing fracture risk, with key risk factors including aging, vitamin D deficiency, sedentary lifestyle, and certain medications. Unlike hyperparathyroidism, which causes elevated parathyroid hormone leading to bone resorption, osteopenia primarily involves reduced bone formation or increased bone loss without the hormonal imbalance. Manifestations include subtle bone weakening and increased susceptibility to fractures, often detected through dual-energy X-ray absorptiometry (DEXA) scans measuring T-scores between -1.0 and -2.5.
Key Differences Between Hyperparathyroidism and Osteopenia
Hyperparathyroidism is a disorder characterized by excessive secretion of parathyroid hormone, leading to increased calcium levels in the blood and bone resorption, whereas osteopenia involves reduced bone mineral density without abnormal hormone levels. Hyperparathyroidism typically causes bone pain, kidney stones, and osteoporosis as complications, while osteopenia primarily increases fracture risk due to decreased bone strength. Diagnosis of hyperparathyroidism relies on elevated serum calcium and parathyroid hormone levels, contrasting with osteopenia, which is identified through decreased bone mineral density on dual-energy X-ray absorptiometry (DEXA) scans.
Pathophysiological Mechanisms: How Each Condition Develops
Hyperparathyroidism results from excessive secretion of parathyroid hormone (PTH), leading to increased bone resorption and calcium mobilization from bones to maintain serum calcium levels. Osteopenia develops due to an imbalance between bone resorption and formation, where bone mineral density decreases without reaching osteoporosis thresholds. The pathophysiology of hyperparathyroidism involves overactive osteoclast activity driven by PTH, whereas osteopenia is primarily caused by reduced bone formation or increased bone loss from factors such as aging, hormonal changes, or nutrient deficiencies.
Diagnostic Approaches for Hyperparathyroidism and Osteopenia
Diagnostic approaches for hyperparathyroidism primarily involve measuring serum calcium and parathyroid hormone (PTH) levels, with elevated calcium and PTH indicating primary hyperparathyroidism. Imaging studies such as sestamibi scans and ultrasound help localize parathyroid adenomas or hyperplasia. Osteopenia diagnosis relies on dual-energy X-ray absorptiometry (DEXA) scans to assess bone mineral density (BMD), with results indicating reduced bone density below normal but not low enough to classify as osteoporosis.
Common Overlapping Symptoms and How to Distinguish Them
Hyperparathyroidism and osteopenia both present with bone-related symptoms such as bone pain, fractures, and reduced bone density, making clinical differentiation challenging. Hyperparathyroidism typically causes elevated serum calcium and parathyroid hormone (PTH) levels, while osteopenia is characterized by decreased bone mineral density without altered calcium or PTH levels. Diagnostic tools including blood tests for calcium and PTH, as well as bone densitometry (DEXA scans), are essential for accurately distinguishing these conditions and guiding appropriate treatment.
Treatment Strategies: Managing Hyperparathyroidism vs Osteopenia
Treatment strategies for hyperparathyroidism focus on surgical intervention such as parathyroidectomy to remove overactive glands, along with medications like bisphosphonates or calcimimetics to regulate calcium levels. Osteopenia management primarily involves lifestyle modifications including increased calcium and vitamin D intake, weight-bearing exercises, and pharmacologic treatments like bisphosphonates to prevent progression to osteoporosis. Monitoring bone mineral density through DEXA scans guides treatment efficacy and adjustment in both conditions.
Impact on Bone Health: Progression and Complications
Hyperparathyroidism causes excessive parathyroid hormone secretion, leading to increased bone resorption and accelerated progression of bone loss, significantly impacting bone density and strength. Osteopenia represents an early stage of decreased bone mineral density but lacks the hormonal imbalance-driven bone remodeling disruptions seen in hyperparathyroidism. Complications of hyperparathyroidism include severe osteoporosis, fractures, and bone deformities, whereas osteopenia primarily increases fracture risk if left untreated.
Preventive Measures and Lifestyle Modifications for Both Conditions
Maintaining adequate calcium and vitamin D intake through diet and supplements is crucial for preventing hyperparathyroidism and osteopenia by supporting bone density and parathyroid function. Regular weight-bearing exercises such as walking, jogging, or resistance training stimulate bone formation and help in managing both conditions effectively. Avoiding smoking and limiting alcohol consumption reduce bone loss and parathyroid gland stress, optimizing long-term skeletal health.
Hyperparathyroidism Infographic
 libterm.com
libterm.com