Strabismus is a condition where the eyes are misaligned, causing them to point in different directions, which can lead to impaired depth perception and double vision. Nystagmus involves involuntary, rhythmic eye movements that can affect visual clarity and balance. Explore this article to understand how these eye disorders impact your vision and the available treatment options.
Table of Comparison
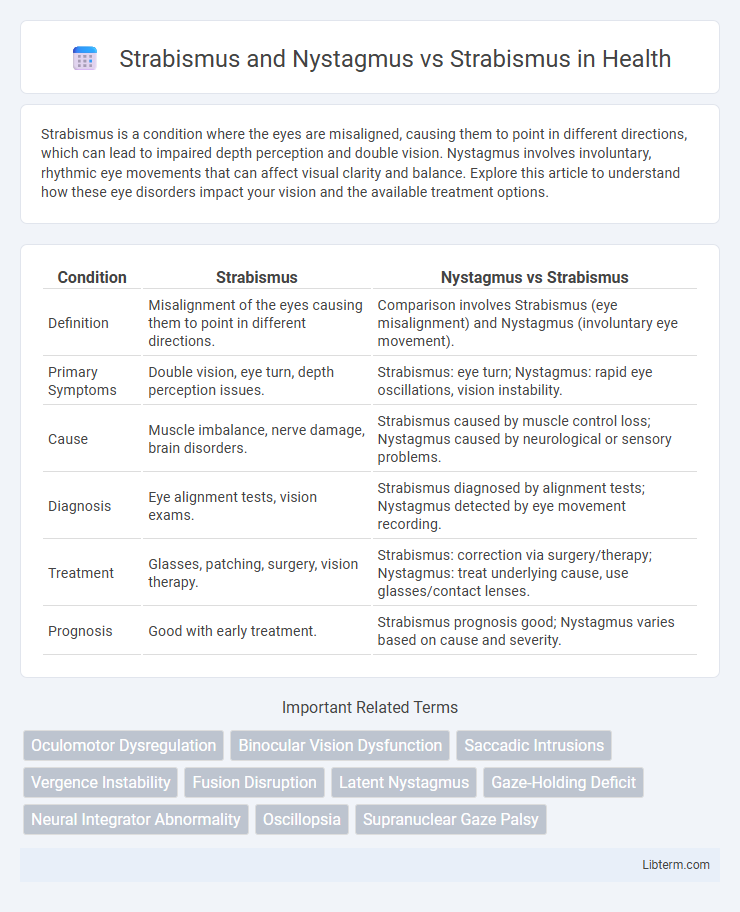
| Condition | Strabismus | Nystagmus vs Strabismus |
|---|---|---|
| Definition | Misalignment of the eyes causing them to point in different directions. | Comparison involves Strabismus (eye misalignment) and Nystagmus (involuntary eye movement). |
| Primary Symptoms | Double vision, eye turn, depth perception issues. | Strabismus: eye turn; Nystagmus: rapid eye oscillations, vision instability. |
| Cause | Muscle imbalance, nerve damage, brain disorders. | Strabismus caused by muscle control loss; Nystagmus caused by neurological or sensory problems. |
| Diagnosis | Eye alignment tests, vision exams. | Strabismus diagnosed by alignment tests; Nystagmus detected by eye movement recording. |
| Treatment | Glasses, patching, surgery, vision therapy. | Strabismus: correction via surgery/therapy; Nystagmus: treat underlying cause, use glasses/contact lenses. |
| Prognosis | Good with early treatment. | Strabismus prognosis good; Nystagmus varies based on cause and severity. |
Understanding Strabismus: Definition and Types
Strabismus is a visual disorder characterized by the misalignment of the eyes, where they do not look in the same direction simultaneously, leading to impaired binocular vision. Nystagmus, often confused with strabismus, involves involuntary, rapid eye movements that affect visual stability rather than alignment. Understanding different types of strabismus, such as esotropia (inward turning) and exotropia (outward turning), is crucial for accurate diagnosis and targeted treatment options.
What is Nystagmus? Causes and Classifications
Nystagmus is a vision condition characterized by involuntary, rapid eye movements that can impair visual stability and focus. Causes of nystagmus include congenital factors, neurological disorders, inner ear problems, and drug toxicity. Classifications of nystagmus comprise congenital nystagmus, manifest latent nystagmus, and acquired nystagmus, each with distinct causes and clinical presentations.
Strabismus and Nystagmus: How Are They Different?
Strabismus is characterized by the misalignment of the eyes, causing one eye to turn inward, outward, upward, or downward, whereas nystagmus involves involuntary, rapid, and repetitive eye movements that can be horizontal, vertical, or rotary. Strabismus primarily affects binocular vision and depth perception, often leading to amblyopia if untreated, while nystagmus impacts visual stability and clarity but does not typically cause eye misalignment. Both conditions require distinct diagnostic approaches and treatments; strabismus often involves corrective lenses, eye exercises, or surgery, while nystagmus management focuses on addressing underlying neurological causes and improving visual function.
Strabismus vs Strabismus with Nystagmus: Clinical Features
Strabismus with nystagmus presents with involuntary eye movements alongside the misalignment characteristic of strabismus alone, complicating visual fixation and depth perception. Patients with both conditions often exhibit reduced visual acuity and poor binocular vision compared to those with isolated strabismus. Clinical features such as alternating esotropia or exotropia coexist with rhythmic oscillations, requiring specialized diagnostic assessments for accurate differentiation and treatment planning.
Symptoms: Strabismus Alone vs Strabismus with Nystagmus
Strabismus alone typically presents with symptoms such as eye misalignment, double vision, and difficulty with depth perception. When strabismus is accompanied by nystagmus, symptoms also include involuntary eye movements, which can cause additional visual disturbances like blurred vision and increased difficulty maintaining steady fixation. This combination often leads to greater challenges in binocular vision and visual stability compared to strabismus without nystagmus.
Diagnosis: Evaluating Strabismus and Nystagmus
Diagnosing strabismus and nystagmus requires comprehensive eye examinations including visual acuity tests, cover-uncover tests, and gaze assessments to observe misalignment and eye movements. Strabismus diagnosis involves identifying the direction and extent of ocular deviation, while nystagmus diagnosis focuses on characterizing involuntary rhythmic eye movements and their triggers. Advanced diagnostic tools such as eye tracking and electrophysiological testing enhance the precision in distinguishing and evaluating these conditions.
Common Causes: Strabismus Only vs Coexisting Conditions
Strabismus primarily results from muscle imbalances, neurological issues, or refractive errors causing misalignment of the eyes, while nystagmus often indicates underlying neurological or sensory impairments and can coexist with strabismus in complex cases. Common causes exclusive to strabismus include congenital muscle abnormalities or cranial nerve dysfunction without involuntary eye oscillations characteristic of nystagmus. When both conditions coexist, they suggest multifactorial etiologies involving central nervous system disorders, genetic syndromes, or sensory deprivation leading to simultaneous ocular misalignment and rhythmic eye movements.
Treatment Approaches: Isolated Strabismus vs Combined Cases
Treatment approaches for isolated strabismus primarily involve corrective measures such as prism glasses, vision therapy, and strabismus surgery to realign the eyes and improve binocular vision. In combined cases of strabismus and nystagmus, management becomes more complex, often requiring a multidisciplinary approach including pharmacological treatments, specialized surgical procedures like tenotomy or Kestenbaum surgery, and low vision aids to address both ocular misalignment and involuntary eye movements. Early intervention and tailored therapies are critical for optimizing visual outcomes and improving quality of life in patients with combined strabismus and nystagmus.
Prognosis: Outcomes for Strabismus vs Strabismus and Nystagmus
Strabismus alone typically has a favorable prognosis when treated early, with many patients achieving significant improvement in eye alignment and binocular vision through corrective surgery or therapy. In contrast, strabismus combined with nystagmus often presents a more complex clinical challenge, as nystagmus can impair visual acuity and stability, potentially limiting the effectiveness of standard strabismus interventions. Long-term outcomes in patients with both conditions may include persistent misalignment and reduced visual function despite optimized management strategies.
Living with Strabismus or Strabismus with Nystagmus: Tips for Patients
Living with strabismus or strabismus combined with nystagmus presents unique challenges such as double vision and involuntary eye movements that affect depth perception and reading ability. Patients benefit from consistent eye exercises, vision therapy, and adaptive techniques like using prism glasses or specialized lenses to improve alignment and reduce symptoms. Regular monitoring by an ophthalmologist ensures timely adjustments to treatment plans, enhancing quality of life and visual function.
Strabismus and Nystagmus Infographic
 libterm.com
libterm.com