Cluster technology optimizes data management by grouping similar data points for faster processing and improved scalability. This approach enhances system performance and reliability, making it essential for business analytics and big data applications. Explore the rest of the article to understand how clusters can transform your data strategy.
Table of Comparison
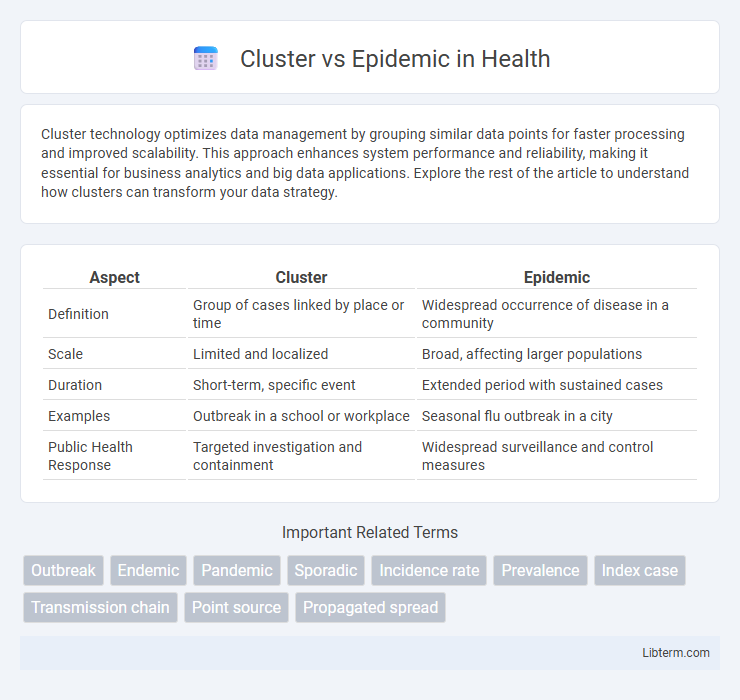
| Aspect | Cluster | Epidemic |
|---|---|---|
| Definition | Group of cases linked by place or time | Widespread occurrence of disease in a community |
| Scale | Limited and localized | Broad, affecting larger populations |
| Duration | Short-term, specific event | Extended period with sustained cases |
| Examples | Outbreak in a school or workplace | Seasonal flu outbreak in a city |
| Public Health Response | Targeted investigation and containment | Widespread surveillance and control measures |
Understanding Disease Clusters: Definition and Examples
Disease clusters refer to a higher-than-expected number of health cases occurring within a specific geographic area or population group over a limited period. Unlike epidemics, which involve widespread occurrences of infectious diseases affecting large populations across regions, clusters often highlight localized incidents such as a cancer cluster near industrial sites or asthma spikes in urban neighborhoods. Understanding these definitions aids in targeted public health investigations and resource allocation to identify potential environmental or genetic risk factors.
What Constitutes an Epidemic? Key Characteristics
An epidemic is characterized by a sudden increase in the number of disease cases within a specific population and geographic area, surpassing the expected baseline incidence. It involves widespread transmission and affects a larger number of individuals compared to a cluster, which refers to a localized, small grouping of cases often confined to a particular place or time. Key characteristics of an epidemic include rapid spread, significant public health impact, and potential to overwhelm healthcare resources.
Cluster vs Epidemic: Core Differences
A cluster refers to a localized, often small group of disease cases occurring in a specific time and place without necessarily exceeding expected baseline levels, while an epidemic signifies a widespread increase in cases beyond normal expectations within a population. Clusters are typically limited in scope and may or may not indicate a broader outbreak, whereas epidemics involve sustained, rapid transmission affecting larger communities or regions. Understanding the distinction aids public health officials in determining the scale and urgency of intervention strategies.
Causes Behind Disease Clusters
Disease clusters refer to a higher-than-expected number of cases occurring within a specific geographic area or population over a short period, often caused by localized environmental exposures, genetic predispositions, or social factors. Epidemics involve a rapid spread of an infectious disease affecting a large number of people across regions, primarily driven by contagious pathogens, lack of immunity, or changes in pathogen virulence. Understanding the causes behind disease clusters requires analyzing environmental toxins, behavioral patterns, or genetic factors, whereas epidemic causes focus on transmission dynamics and population susceptibility.
How Epidemics Spread: Patterns and Triggers
Epidemics spread through complex patterns involving person-to-person transmission, environmental factors, and social behavior, often triggered by high population density, poor sanitation, and travel. Clusters represent localized, concentrated cases confined to specific areas, while epidemics extend more broadly, crossing communities and regions. Understanding transmission vectors, incubation periods, and immunity levels helps map epidemic trajectories and implement timely control measures.
Surveillance Methods for Clusters and Epidemics
Surveillance methods for clusters involve localized case identification and detailed contact tracing to detect concentrated outbreaks within specific populations or areas, employing tools such as spatial mapping and case definition refinement. Epidemic surveillance relies on broader, population-level data collection including syndromic surveillance, real-time reporting systems, and statistical models to monitor widespread and rapidly spreading disease incidence. Combining laboratory diagnostics with digital health records enhances both cluster detection and epidemic tracking by providing accurate case confirmation and trend analysis.
Public Health Response: Cluster vs Epidemic
Public health response to a cluster involves targeted investigations and localized interventions to contain and prevent further spread within a specific community or setting. In contrast, epidemic response requires broader strategies including widespread surveillance, resource allocation, and public communication to manage disease spread on a larger scale. Rapid identification, contact tracing, and vaccination campaigns are crucial for both, but the scale and coordination differ significantly between clusters and epidemics.
Case Studies: Notable Clusters and Epidemics
Notable case studies reveal that clusters often represent localized outbreaks, such as the SARS outbreak in a Hong Kong hospital where transmission occurred among healthcare workers and patients. In contrast, epidemics, like the 2014-2016 West Africa Ebola epidemic, involve widespread transmission across multiple regions, significantly impacting public health systems and requiring large-scale containment strategies. Detailed epidemiological analysis of clusters and epidemics enhances understanding of transmission dynamics, informing targeted interventions and resource allocation.
Challenges in Identifying Clusters and Epidemics
Identifying clusters involves detecting a localized, irregular increase in disease incidence within a specific population or area, often complicated by limited data, underreporting, and variability in case definitions. Epidemic identification requires recognizing a widespread, significant rise in disease occurrence exceeding the expected baseline across larger regions, challenged by delayed reporting, heterogeneous transmission dynamics, and the influence of environmental or social factors. Differentiating between clusters and epidemics relies heavily on robust surveillance systems, precise epidemiological criteria, and timely data analysis to inform public health responses.
Prevention Strategies for Future Outbreaks
Effective prevention strategies for future outbreaks emphasize early detection and containment of clusters to prevent progression into epidemics. Implementing robust surveillance systems, widespread testing, and targeted quarantine measures can limit transmission within localized clusters. Public health education and vaccination campaigns further strengthen community immunity, reducing the risk of widespread epidemic spread.
Cluster Infographic
 libterm.com
libterm.com