Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition characterized by persistent airflow limitation and breathing difficulties caused primarily by long-term exposure to irritants such as cigarette smoke. Symptoms often include chronic cough, mucus production, and shortness of breath, significantly impacting quality of life and requiring ongoing medical management. Discover effective strategies and treatments to help you manage COPD by reading the full article.
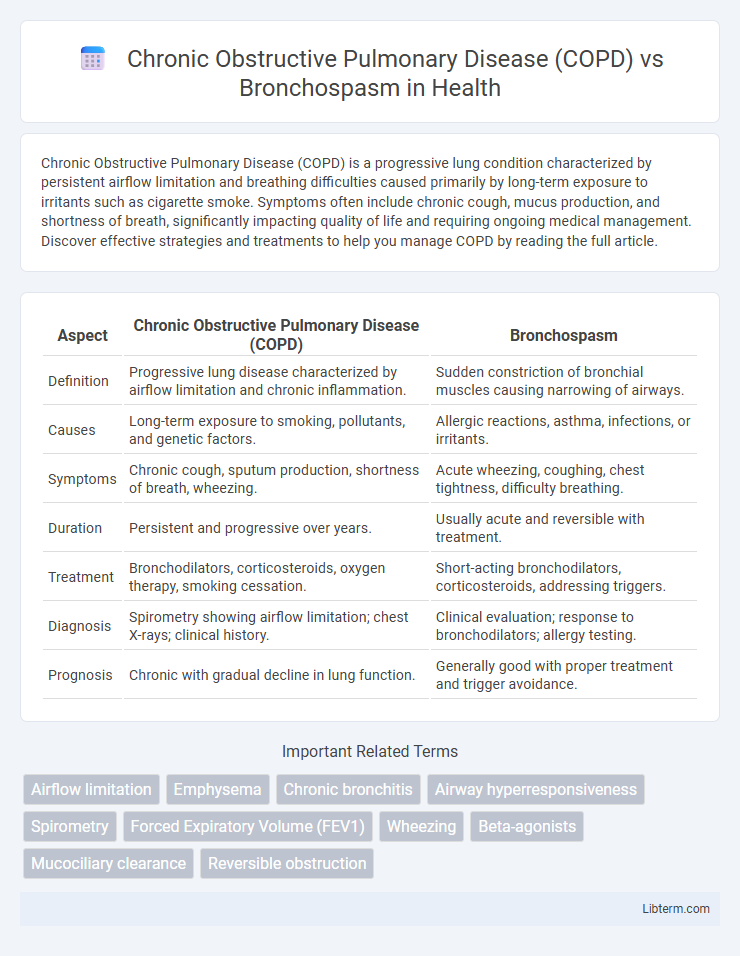
Table of Comparison
| Aspect | Chronic Obstructive Pulmonary Disease (COPD) | Bronchospasm |
|---|---|---|
| Definition | Progressive lung disease characterized by airflow limitation and chronic inflammation. | Sudden constriction of bronchial muscles causing narrowing of airways. |
| Causes | Long-term exposure to smoking, pollutants, and genetic factors. | Allergic reactions, asthma, infections, or irritants. |
| Symptoms | Chronic cough, sputum production, shortness of breath, wheezing. | Acute wheezing, coughing, chest tightness, difficulty breathing. |
| Duration | Persistent and progressive over years. | Usually acute and reversible with treatment. |
| Treatment | Bronchodilators, corticosteroids, oxygen therapy, smoking cessation. | Short-acting bronchodilators, corticosteroids, addressing triggers. |
| Diagnosis | Spirometry showing airflow limitation; chest X-rays; clinical history. | Clinical evaluation; response to bronchodilators; allergy testing. |
| Prognosis | Chronic with gradual decline in lung function. | Generally good with proper treatment and trigger avoidance. |
Understanding Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disorder characterized by persistent airflow limitation and chronic inflammation in the airways and alveoli, resulting primarily from long-term exposure to irritants such as cigarette smoke. Unlike bronchospasm, which is a temporary constriction of the bronchial muscles causing acute airflow obstruction, COPD involves structural lung damage including emphysema and chronic bronchitis that impair gas exchange over time. Effective management of COPD requires a combination of bronchodilators, corticosteroids, and lifestyle changes aimed at reducing symptoms, preventing exacerbations, and improving overall lung function.
Defining Bronchospasm: Causes and Symptoms
Bronchospasm is the sudden constriction of the muscles in the walls of the bronchioles, leading to narrowing of the airways and difficulty breathing. Common causes include asthma, allergic reactions, respiratory infections, and exposure to irritants such as smoke or pollutants. Symptoms typically involve wheezing, coughing, shortness of breath, and chest tightness, distinguishing bronchospasm from the progressive airflow limitation characteristic of Chronic Obstructive Pulmonary Disease (COPD).
Key Differences Between COPD and Bronchospasm
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disorder characterized by persistent airflow limitation due to chronic inflammation and structural damage, primarily caused by long-term exposure to irritants such as cigarette smoke. Bronchospasm refers to the sudden constriction of bronchial smooth muscle, leading to reversible airway narrowing often triggered by asthma, allergies, or irritants, resulting in acute symptoms like wheezing and shortness of breath. Unlike COPD's chronic, irreversible airflow obstruction, bronchospasm is typically transient and reversible with bronchodilator treatment, highlighting a fundamental difference in pathophysiology and management approaches.
Common Risk Factors for COPD and Bronchospasm
Common risk factors for Chronic Obstructive Pulmonary Disease (COPD) include long-term exposure to cigarette smoke, occupational dust, and chemical fumes, along with a history of respiratory infections and genetic predisposition such as alpha-1 antitrypsin deficiency. Bronchospasm, often triggered by asthma, allergies, or respiratory irritants, shares overlapping risk elements with COPD, such as tobacco smoke exposure and air pollution. Both conditions are exacerbated by environmental pollutants, respiratory infections, and personal behaviors that impair airway function and increase inflammation.
Recognizing Symptoms: COPD vs Bronchospasm
Chronic Obstructive Pulmonary Disease (COPD) presents with persistent symptoms such as chronic cough, sputum production, and progressive shortness of breath, often worsening over months or years. Bronchospasm, characterized by sudden constriction of airway muscles, results in acute wheezing, chest tightness, and rapid onset dyspnea. Differentiating COPD from bronchospasm involves assessing symptom duration, with COPD showing chronic progression and bronchospasm demonstrating episodic, often reversible airflow obstruction.
Diagnostic Approaches: COPD Compared to Bronchospasm
Diagnostic approaches for Chronic Obstructive Pulmonary Disease (COPD) primarily involve spirometry to measure airflow limitation and assess the degree of airway obstruction, often revealing reduced FEV1/FVC ratios. In contrast, bronchospasm diagnosis typically relies on clinical evaluation, peak flow measurements, and response to bronchodilators, as the reversible airway constriction differentiates it from the persistent obstruction seen in COPD. Imaging studies such as chest X-rays or CT scans may support COPD diagnosis by identifying emphysema or airway wall thickening, whereas these are not definitive in isolated bronchospasm cases.
Treatment Strategies for COPD
Treatment strategies for Chronic Obstructive Pulmonary Disease (COPD) primarily involve bronchodilators such as long-acting beta2-agonists (LABAs) and long-acting muscarinic antagonists (LAMAs) to improve airflow and reduce symptoms. Inhaled corticosteroids (ICS) are often combined with bronchodilators to manage inflammation and reduce exacerbations in moderate to severe cases. Pulmonary rehabilitation, oxygen therapy, and smoking cessation are essential components of comprehensive COPD management to enhance lung function and quality of life.
Effective Management of Bronchospasm
Effective management of bronchospasm, a common symptom in Chronic Obstructive Pulmonary Disease (COPD), involves rapid bronchodilation through short-acting beta2-agonists (SABAs) such as albuterol and anticholinergics like ipratropium. Inhaled corticosteroids may be used to reduce airway inflammation, improving overall lung function and decreasing exacerbation frequency. Long-term treatment strategies emphasize personalized pharmacotherapy, pulmonary rehabilitation, and lifestyle modifications to control bronchospasm episodes and enhance patient quality of life.
Preventive Measures for Both Conditions
Preventive measures for Chronic Obstructive Pulmonary Disease (COPD) include smoking cessation, avoidance of environmental pollutants, and vaccination against influenza and pneumococcal infections to reduce exacerbations. Bronchospasm prevention involves minimizing exposure to triggers such as allergens, irritants, and respiratory infections, along with adherence to prescribed bronchodilator therapy and use of inhaled corticosteroids when indicated. Both conditions benefit from maintaining good respiratory hygiene and regular medical follow-up to monitor lung function and manage symptoms effectively.
Living With Chronic Lung Disease: Support and Resources
Living with Chronic Obstructive Pulmonary Disease (COPD) requires comprehensive support systems including pulmonary rehabilitation, oxygen therapy, and access to specialized healthcare providers to manage symptoms and improve quality of life. Bronchospasm, often triggered by asthma or COPD exacerbations, necessitates rapid intervention with bronchodilators and anti-inflammatory medications to prevent worsening respiratory function. Patient education, support groups, and community resources play a critical role in helping individuals navigate daily challenges and maintain lung health.
Chronic Obstructive Pulmonary Disease (COPD) Infographic
 libterm.com
libterm.com