Maintaining euhydration ensures your body's optimal fluid balance, supporting vital functions such as temperature regulation, nutrient transport, and cognitive performance. Proper hydration enhances physical endurance and prevents dehydration-related complications like headaches and fatigue. Discover essential tips and strategies to achieve and maintain euhydration throughout the day in the rest of this article.
Table of Comparison
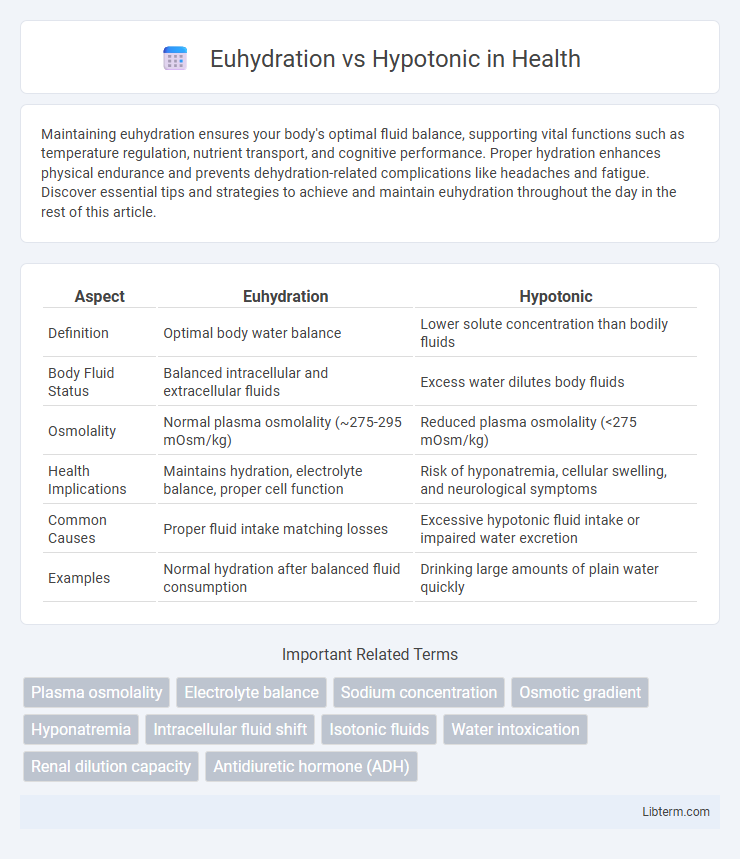
| Aspect | Euhydration | Hypotonic |
|---|---|---|
| Definition | Optimal body water balance | Lower solute concentration than bodily fluids |
| Body Fluid Status | Balanced intracellular and extracellular fluids | Excess water dilutes body fluids |
| Osmolality | Normal plasma osmolality (~275-295 mOsm/kg) | Reduced plasma osmolality (<275 mOsm/kg) |
| Health Implications | Maintains hydration, electrolyte balance, proper cell function | Risk of hyponatremia, cellular swelling, and neurological symptoms |
| Common Causes | Proper fluid intake matching losses | Excessive hypotonic fluid intake or impaired water excretion |
| Examples | Normal hydration after balanced fluid consumption | Drinking large amounts of plain water quickly |
Introduction to Euhydration and Hypotonic States
Euhydration refers to the optimal state of body water balance where fluid intake equals fluid loss, maintaining physiological functions and cellular homeostasis. Hypotonic states occur when extracellular fluid has a lower concentration of solutes than intracellular fluid, causing water to move into cells and potentially leading to cellular swelling and electrolyte imbalances. Understanding the distinction between euhydration and hypotonic conditions is crucial for managing hydration strategies in clinical and athletic settings.
Defining Euhydration: Optimal Body Water Balance
Euhydration refers to the state of optimal body water balance where fluid intake matches fluid loss, maintaining cellular function and physiological processes. It ensures adequate hydration without causing cellular swelling or dehydration, sustaining normal blood volume and electrolyte concentrations. In contrast, hypotonic conditions involve lower solute concentration than body fluids, potentially leading to cellular overhydration and electrolyte imbalance.
What is Hypotonic? Understanding Fluid Imbalances
Hypotonic refers to a fluid state where the concentration of solutes outside the cells is lower than inside, causing water to move into cells and potentially leading to swelling or cellular dysfunction. This imbalance disrupts normal hydration levels and can result from excessive water intake, certain medical conditions, or electrolyte imbalances. Understanding hypotonic conditions is essential for managing fluid therapy and preventing complications like hyponatremia or edema.
Physiological Importance of Euhydration
Euhydration maintains optimal intracellular and extracellular fluid balance, which is essential for cellular function, thermoregulation, and cardiovascular stability. In contrast, hypotonic conditions can lead to cellular swelling and electrolyte imbalances, impairing muscle function and neurological performance. Sustaining euhydration supports metabolic efficiency and enhances physical endurance by preventing dehydration-related declines in blood plasma volume and thermoregulatory capacity.
Causes and Consequences of Hypotonic Hydration
Hypotonic hydration occurs when excessive water intake dilutes blood sodium levels, causing an imbalance known as hyponatremia. This condition can result from vigorous exercise with high water consumption or medical issues like kidney problems, leading to symptoms such as headache, nausea, confusion, and in severe cases, cerebral edema and seizures. Maintaining euhydration ensures proper electrolyte balance and optimal cellular function, preventing the dangerous effects associated with hypotonic hydration.
Comparing Symptoms: Euhydration vs Hypotonic State
Euhydration maintains normal fluid balance with symptoms such as stable heart rate, clear cognition, and normal urine output, while hypotonic state presents with symptoms like headache, nausea, muscle cramps, and confusion due to cellular swelling from low plasma osmolality. In euhydration, electrolyte levels remain balanced, preventing neurological disturbances, but hypotonic conditions often lead to hyponatremia and impaired neuromuscular function. Early recognition of these contrasting symptoms is critical for accurate diagnosis and appropriate intervention to restore fluid and electrolyte homeostasis.
Fluid Intake Recommendations and Risks
Euhydration maintains optimal fluid balance by matching water intake with losses, supporting physiological functions and performance. Hypotonic fluid intake, which contains lower solute concentrations than body fluids, rapidly replenishes water but risks diluting electrolytes if consumed excessively. Recommendations emphasize consuming hypotonic fluids during prolonged exercise to prevent dehydration while avoiding overhydration that can lead to hyponatremia and associated health complications.
Diagnosing Hydration Status: Key Indicators
Euhydration is characterized by balanced fluid levels, with key diagnostic indicators including stable plasma osmolality around 280-295 mOsm/kg and normal urine specific gravity below 1.020. Hypotonic hydration involves excess water relative to electrolytes, presenting with low plasma osmolality under 275 mOsm/kg and dilute urine with specific gravity under 1.005. Accurate diagnosis depends on assessing serum sodium concentration, urine output, and clinical symptoms to distinguish between optimal and diluted hydration statuses.
Preventing Hypotonic Complications in Athletes
Maintaining euhydration is essential for athletes to prevent hypotonic complications such as hyponatremia, which occurs when excessive water intake dilutes blood sodium levels. Strategies include tailored fluid replacement based on sweat rate, electrolyte-enhanced beverages, and monitoring body weight changes pre- and post-exercise. Proper hydration protocols reduce the risk of cellular swelling and neurological symptoms, ensuring optimal performance and safety during intense physical activity.
Conclusion: Striking the Right Hydration Balance
Maintaining euhydration versus consuming hypotonic fluids hinges on the body's precise fluid and electrolyte needs during physical activity. Euhydration supports optimal physiological function by preserving cellular balance and preventing dehydration, while hypotonic solutions aid rapid fluid absorption with minimal electrolyte disruption. Striking the right hydration balance involves assessing individual sweat rate, exercise intensity, and duration to select appropriate fluid types and volumes for sustained performance and recovery.
Euhydration Infographic
 libterm.com
libterm.com