Hemorrhage refers to the excessive or uncontrolled bleeding that occurs when blood vessels are damaged. Prompt identification and treatment are crucial to prevent severe complications or life-threatening situations. Discover more about symptoms, causes, and treatment options to protect Your health in the article ahead.
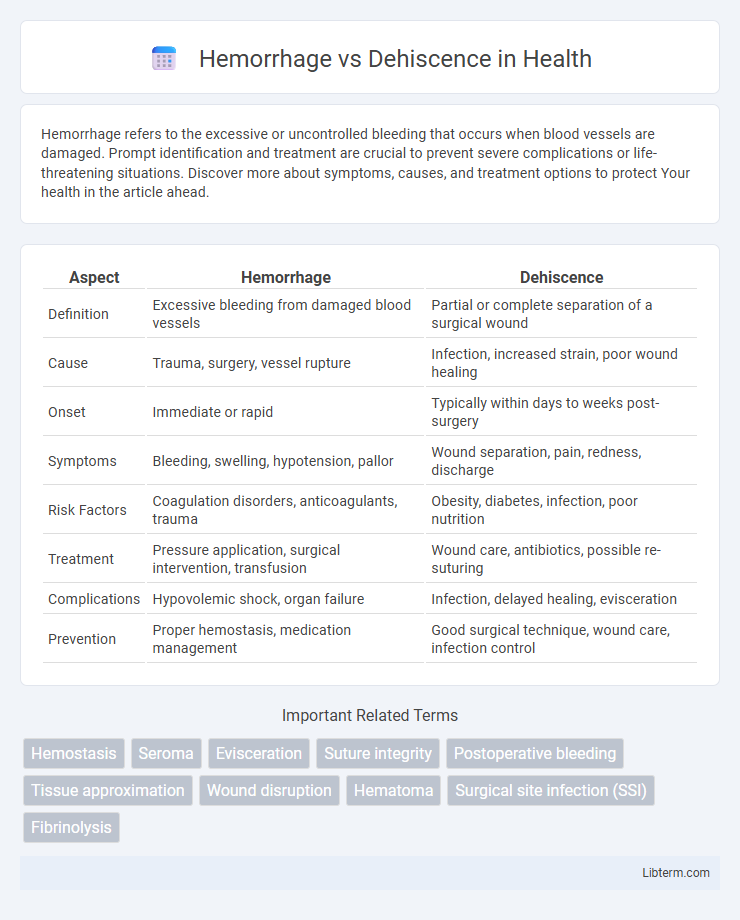
Table of Comparison
| Aspect | Hemorrhage | Dehiscence |
|---|---|---|
| Definition | Excessive bleeding from damaged blood vessels | Partial or complete separation of a surgical wound |
| Cause | Trauma, surgery, vessel rupture | Infection, increased strain, poor wound healing |
| Onset | Immediate or rapid | Typically within days to weeks post-surgery |
| Symptoms | Bleeding, swelling, hypotension, pallor | Wound separation, pain, redness, discharge |
| Risk Factors | Coagulation disorders, anticoagulants, trauma | Obesity, diabetes, infection, poor nutrition |
| Treatment | Pressure application, surgical intervention, transfusion | Wound care, antibiotics, possible re-suturing |
| Complications | Hypovolemic shock, organ failure | Infection, delayed healing, evisceration |
| Prevention | Proper hemostasis, medication management | Good surgical technique, wound care, infection control |
Introduction to Hemorrhage and Dehiscence
Hemorrhage refers to excessive or uncontrolled bleeding, either internal or external, caused by trauma, surgical complications, or underlying medical conditions. Dehiscence is the partial or complete separation of a surgical wound or incision, often resulting from infection, poor wound healing, or mechanical stress. Both complications require prompt medical assessment to prevent severe outcomes and facilitate appropriate treatment.
Definitions and Key Differences
Hemorrhage is the excessive or uncontrolled bleeding from blood vessels due to injury or surgery, while dehiscence refers to the partial or complete separation of a surgical wound or incision. Key differences include hemorrhage involving blood loss and cardiovascular risk, whereas dehiscence compromises wound integrity and increases infection risk. Hemorrhage requires immediate hemostatic management, whereas dehiscence often necessitates wound care and possible surgical intervention.
Causes of Hemorrhage in Surgical Patients
Hemorrhage in surgical patients primarily results from arterial or venous injury during incision, inadequate hemostasis, or vessel erosion caused by infection or foreign bodies. Coagulopathy, hypertension, and use of anticoagulant medications further increase bleeding risk by impairing normal clot formation and vessel constriction. Understanding these causes is critical for surgical teams to implement effective bleeding control measures and reduce postoperative complications.
Causes of Dehiscence After Surgery
Dehiscence after surgery commonly results from factors such as poor wound healing due to infection, inadequate surgical technique, or excessive tension on the wound edges. Patient-related causes include malnutrition, diabetes, obesity, and the use of corticosteroids or immunosuppressive medications, all of which impair tissue regeneration. Identifying these risk factors is crucial to prevent wound separation and subsequent complications like hemorrhage or infection.
Clinical Signs and Symptoms
Hemorrhage presents with clinical signs such as rapid swelling, pallor, hypotension, and tachycardia indicating significant blood loss. Dehiscence typically manifests through symptoms including sudden wound opening, serosanguinous drainage, localized pain, and increased separation of wound edges. Both conditions require prompt clinical assessment to prevent complications like infection, shock, or delayed healing.
Risk Factors for Hemorrhage and Dehiscence
Risk factors for hemorrhage include hypertension, anticoagulant therapy, trauma, and coagulation disorders, which increase the likelihood of excessive bleeding. Dehiscence risk factors involve poor surgical technique, infection, malnutrition, diabetes, and excessive tension on wound edges, all contributing to the premature separation of a surgical incision. Both conditions require meticulous management of these risk factors to promote optimal healing and prevent complications.
Diagnostic Approaches
Diagnostic approaches for hemorrhage primarily involve clinical assessment combined with imaging techniques such as ultrasound, CT scan, or MRI to identify the source and extent of bleeding. Dehiscence diagnosis relies on physical examination and imaging studies like ultrasound or CT to detect wound separation or gap formation, often supported by laboratory tests to assess infection or inflammation markers. Both conditions may require endoscopic evaluation or surgical exploration for definitive diagnosis and treatment planning.
Prevention Strategies
Effective prevention strategies for hemorrhage include meticulous surgical technique to ensure proper vessel ligation and use of hemostatic agents, while continuous monitoring of coagulation status in patients is critical. To prevent wound dehiscence, maintaining optimal nutritional status, controlling blood glucose levels, and employing appropriate suture materials with tension-reducing techniques can significantly improve wound integrity. Use of prophylactic antibiotics and ensuring adequate wound care further reduce infection risk, which is a key factor in both hemorrhage and dehiscence prevention.
Management and Treatment Options
Hemorrhage management involves immediate hemostasis through direct pressure, surgical intervention, or use of hemostatic agents, supported by blood transfusions and fluid resuscitation to maintain hemodynamic stability. Dehiscence treatment includes wound care with aseptic dressing, antibiotics to prevent infection, and surgical re-closure or reinforcement depending on the severity and underlying cause. Both conditions require close monitoring and tailored approaches based on the patient's overall health and wound characteristics.
Prognosis and Patient Outcomes
Hemorrhage after surgery can lead to significant morbidity due to blood loss and compromised tissue oxygenation, often requiring urgent intervention to prevent shock and organ failure. Dehiscence, the partial or complete separation of a surgical wound, increases the risk of infection and prolonged hospitalization, negatively impacting patient recovery and long-term outcomes. Prognosis for hemorrhage depends on prompt hemostasis, while dehiscence prognosis hinges on timely wound management and prevention of secondary complications such as sepsis.
Hemorrhage Infographic
 libterm.com
libterm.com