Hypoglycemia occurs when blood sugar levels drop below normal, causing symptoms like shaking, sweating, confusion, and dizziness. Managing this condition involves monitoring your glucose levels closely and taking immediate action to raise your blood sugar if needed. Discover how to effectively recognize, prevent, and treat hypoglycemia by reading the rest of the article.
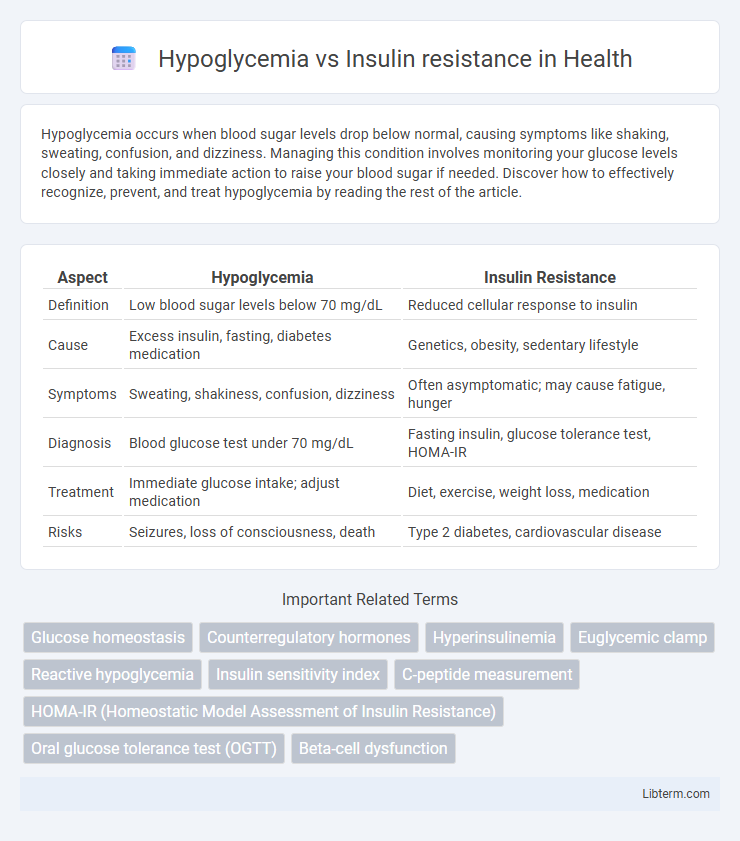
Table of Comparison
| Aspect | Hypoglycemia | Insulin Resistance |
|---|---|---|
| Definition | Low blood sugar levels below 70 mg/dL | Reduced cellular response to insulin |
| Cause | Excess insulin, fasting, diabetes medication | Genetics, obesity, sedentary lifestyle |
| Symptoms | Sweating, shakiness, confusion, dizziness | Often asymptomatic; may cause fatigue, hunger |
| Diagnosis | Blood glucose test under 70 mg/dL | Fasting insulin, glucose tolerance test, HOMA-IR |
| Treatment | Immediate glucose intake; adjust medication | Diet, exercise, weight loss, medication |
| Risks | Seizures, loss of consciousness, death | Type 2 diabetes, cardiovascular disease |
Understanding Hypoglycemia: Definition and Causes
Hypoglycemia is a condition characterized by abnormally low blood glucose levels, typically below 70 mg/dL, leading to symptoms such as shakiness, sweating, confusion, and in severe cases, loss of consciousness. Causes of hypoglycemia include excessive insulin administration in diabetic patients, prolonged fasting, certain medications, hormone deficiencies, and critical illnesses affecting the liver or kidneys. Understanding the underlying factors of hypoglycemia is essential for differentiating it from insulin resistance, which involves impaired cellular response to insulin and often results in elevated blood sugar levels rather than low glucose.
What is Insulin Resistance?
Insulin resistance occurs when the body's cells respond poorly to insulin, leading to impaired glucose uptake and elevated blood sugar levels. This metabolic condition often precedes type 2 diabetes and is associated with obesity, high triglycerides, and hypertension. Unlike hypoglycemia, which involves abnormally low blood glucose, insulin resistance results in chronic hyperglycemia due to ineffective insulin action.
Key Differences Between Hypoglycemia and Insulin Resistance
Hypoglycemia is characterized by abnormally low blood glucose levels, often resulting in symptoms like dizziness, sweating, and confusion, whereas insulin resistance involves the diminished ability of cells to respond to insulin, leading to elevated blood sugar and potential progression to type 2 diabetes. Hypoglycemia typically requires immediate glucose intake to restore blood sugar levels, while insulin resistance necessitates lifestyle changes, medications, and management of underlying metabolic conditions. The diagnostic criteria also differ, with hypoglycemia confirmed by blood glucose levels below 70 mg/dL, and insulin resistance assessed through markers like fasting insulin, HOMA-IR, or glucose tolerance tests.
Common Symptoms: Hypoglycemia vs Insulin Resistance
Hypoglycemia commonly presents with symptoms such as shakiness, sweating, confusion, and dizziness due to low blood sugar levels. Insulin resistance often manifests through symptoms like increased hunger, fatigue, and difficulty concentrating, reflecting impaired cellular glucose uptake. Both conditions may share overlapping signs like irritability and headaches, but their underlying biochemical causes differ significantly.
Diagnostic Methods for Each Condition
Hypoglycemia diagnosis relies heavily on measuring blood glucose levels during symptomatic episodes, often confirmed by a supervised fasting test or continuous glucose monitoring. Insulin resistance is primarily assessed through the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) or oral glucose tolerance tests (OGTT), which evaluate insulin response and glucose metabolism. Advanced techniques like hyperinsulinemic-euglycemic clamps provide precise insulin sensitivity measurements but are typically reserved for research settings.
Risk Factors Associated with Hypoglycemia and Insulin Resistance
Risk factors associated with hypoglycemia include excessive insulin administration, prolonged fasting, certain medications such as sulfonylureas, and underlying conditions like renal failure or adrenal insufficiency. Insulin resistance is primarily linked to obesity, physical inactivity, genetic predisposition, and metabolic syndrome components including hypertension and dyslipidemia. Both conditions are influenced by dietary patterns, stress levels, and chronic illnesses, which exacerbate glucose metabolism disturbances.
Impact on Metabolic Health
Hypoglycemia causes sudden drops in blood glucose levels, leading to impaired brain function and triggering stress hormone release, which can disrupt metabolic balance. In contrast, insulin resistance results in chronically elevated blood glucose and insulin levels, promoting inflammation, fat accumulation, and increased risk of type 2 diabetes and cardiovascular disease. Both conditions negatively impact metabolic health but through distinct mechanisms affecting glucose utilization and hormonal regulation.
Prevention Strategies for Hypoglycemia and Insulin Resistance
Preventing hypoglycemia involves regular monitoring of blood glucose levels, consuming balanced meals with complex carbohydrates, and avoiding excessive insulin or medication dosages. Insulin resistance prevention emphasizes maintaining a healthy weight, engaging in regular physical activity, and adopting a diet rich in fiber, whole grains, and low in processed sugars. Both conditions benefit from consistent lifestyle modifications tailored to individual metabolic responses and medical guidance.
Treatment Approaches: Managing Symptoms and Causes
Hypoglycemia treatment involves quick administration of fast-acting carbohydrates to raise blood glucose levels and prevent severe symptoms, alongside long-term dietary adjustments to maintain stable sugar levels. Insulin resistance management focuses on lifestyle modifications such as weight loss, regular physical activity, and a balanced diet low in refined sugars to enhance cellular response to insulin. Pharmacological interventions like metformin are often prescribed to improve insulin sensitivity and control blood glucose, addressing the root cause rather than just symptoms.
Long-Term Health Implications and Lifestyle Considerations
Hypoglycemia involves dangerously low blood sugar levels, posing risks such as cognitive impairment and seizures if untreated, while insulin resistance is marked by the body's reduced ability to use insulin effectively, often leading to type 2 diabetes and cardiovascular complications. Long-term health implications of insulin resistance include increased risk of metabolic syndrome, chronic inflammation, and organ damage, whereas recurrent hypoglycemia can cause neurological damage and impaired hormone function. Lifestyle modifications for managing insulin resistance focus on a balanced diet, regular exercise, and weight control, while hypoglycemia management prioritizes consistent meal timing, carbohydrate intake monitoring, and avoiding fasting or intense physical activity without proper glucose levels.
Hypoglycemia Infographic
 libterm.com
libterm.com