A transient ischemic attack (TIA) occurs when there is a temporary disruption of blood flow to the brain, causing stroke-like symptoms that usually last less than 24 hours. Recognizing the signs of a TIA is crucial because it serves as a warning for potential future strokes and prompts immediate medical evaluation to reduce your risk. Discover more about the causes, symptoms, and prevention strategies in the rest of this article.
Table of Comparison
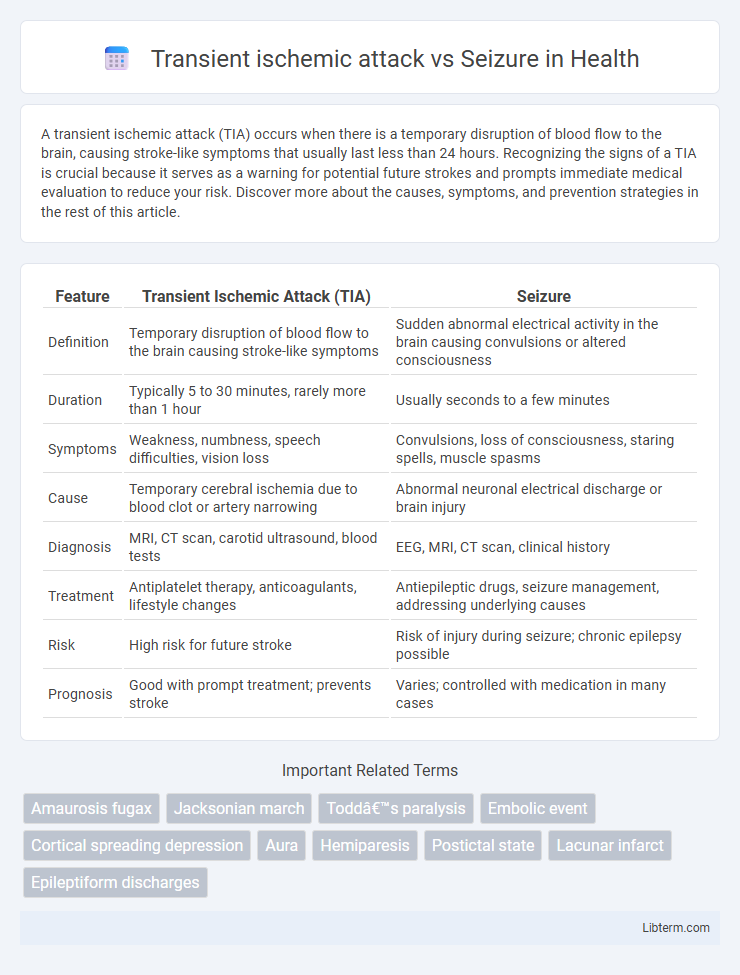
| Feature | Transient Ischemic Attack (TIA) | Seizure |
|---|---|---|
| Definition | Temporary disruption of blood flow to the brain causing stroke-like symptoms | Sudden abnormal electrical activity in the brain causing convulsions or altered consciousness |
| Duration | Typically 5 to 30 minutes, rarely more than 1 hour | Usually seconds to a few minutes |
| Symptoms | Weakness, numbness, speech difficulties, vision loss | Convulsions, loss of consciousness, staring spells, muscle spasms |
| Cause | Temporary cerebral ischemia due to blood clot or artery narrowing | Abnormal neuronal electrical discharge or brain injury |
| Diagnosis | MRI, CT scan, carotid ultrasound, blood tests | EEG, MRI, CT scan, clinical history |
| Treatment | Antiplatelet therapy, anticoagulants, lifestyle changes | Antiepileptic drugs, seizure management, addressing underlying causes |
| Risk | High risk for future stroke | Risk of injury during seizure; chronic epilepsy possible |
| Prognosis | Good with prompt treatment; prevents stroke | Varies; controlled with medication in many cases |
Understanding Transient Ischemic Attack (TIA): An Overview
Transient ischemic attack (TIA) is a brief neurological dysfunction caused by a temporary disruption of blood flow to the brain, often lasting less than 24 hours and resolving without permanent damage. Unlike seizures, which result from abnormal electrical activity in the brain, TIAs are primarily vascular events indicating a high risk of stroke. Recognizing the defining clinical features of TIA, such as sudden weakness, numbness, or speech difficulties, is critical for timely diagnosis and prevention of subsequent cerebrovascular incidents.
Seizures Explained: Causes and Types
Seizures result from abnormal electrical activity in the brain, with causes ranging from epilepsy, brain injury, infections, and metabolic imbalances to genetic factors. Types of seizures include focal seizures, affecting one part of the brain, and generalized seizures, which involve the entire brain and manifest as convulsions or loss of consciousness. Differentiating seizures from transient ischemic attacks (TIAs) is critical, as TIAs are temporary disruptions of blood flow to the brain, not electrical disturbances.
Key Differences Between TIA and Seizure
Transient ischemic attack (TIA) involves a temporary blockage of blood flow to the brain causing stroke-like symptoms lasting less than 24 hours, while a seizure is an abnormal electrical discharge in the brain resulting in convulsions or altered consciousness. TIAs generally present with sudden unilateral weakness, numbness, or speech difficulties without loss of consciousness, whereas seizures may include loss of consciousness, muscle spasms, and postictal confusion. Diagnostic differentiation relies on neuroimaging and EEG, with TIAs showing no epileptiform activity and seizures often confirmed by abnormal EEG patterns.
Clinical Presentation: Symptoms of TIA vs Seizure
Transient ischemic attack (TIA) presents with sudden, focal neurological deficits such as unilateral weakness, numbness, speech difficulties, vision changes, or dizziness, typically resolving within minutes to hours without lasting damage. Seizures often manifest with abnormal motor activity, such as convulsions, loss of consciousness, sensory disturbances, or automatisms, and may include postictal confusion or fatigue. Unlike TIAs, seizures usually involve rhythmic, involuntary movements and can affect consciousness unpredictably.
Risk Factors: Who Is at Risk for TIA and Seizure?
Risk factors for transient ischemic attack (TIA) primarily include hypertension, diabetes, smoking, atrial fibrillation, and a history of cardiovascular disease, increasing the likelihood of cerebrovascular events. Seizure risk factors encompass epilepsy, brain injury, infections, and metabolic disturbances, with heightened susceptibility in individuals with neurological disorders or a family history of seizures. Both conditions demand careful risk assessment to implement timely prevention and management strategies.
Diagnosis: How Doctors Differentiate TIA from Seizure
Doctors differentiate transient ischemic attack (TIA) from seizure primarily through detailed patient history and neurological examination, emphasizing symptom onset and duration. Diagnostic tools such as MRI with diffusion-weighted imaging and electroencephalogram (EEG) are critical; MRI detects ischemic changes indicative of TIA, while EEG identifies abnormal electrical activity characteristic of seizures. Blood tests, cardiac evaluation, and vascular imaging further support diagnosis by revealing risk factors for cerebrovascular events or epileptiform activity.
Immediate Management: What to Do During an Episode
During a transient ischemic attack (TIA), immediately call emergency services and keep the person calm while monitoring airway, breathing, and circulation; avoid giving any food or drink. For seizures, ensure the person is safely positioned on their side to maintain airway patency, clear the area of harmful objects, and time the seizure duration without restraining movements. Rapid medical evaluation is critical for both conditions to prevent further neurological damage or complications.
Long-term Treatment and Prevention Strategies
Long-term treatment for transient ischemic attack (TIA) focuses on antiplatelet therapy, blood pressure control, cholesterol management, and lifestyle modifications to reduce stroke risk. Seizure management typically involves antiepileptic drugs tailored to seizure type, regular monitoring, and avoiding triggers to prevent recurrence. Preventive strategies for TIA emphasize addressing vascular risk factors, while seizure prevention depends on adherence to medication and managing underlying neurological conditions.
Prognosis: Outcomes After TIA vs Seizure
Transient ischemic attacks (TIAs) often indicate a higher risk of future ischemic stroke, with prognosis depending heavily on timely intervention and management of underlying vascular risks. Seizures vary widely in outcomes based on etiology, seizure frequency, and response to antiepileptic treatment, but they generally have a lower immediate risk of mortality compared to TIAs. After a TIA, patients require aggressive secondary prevention strategies to improve prognosis, while seizure prognosis improves with proper diagnosis and compliance to treatment regimens.
When to Seek Medical Attention: Recognizing Emergency Signs
Seek immediate medical attention if sudden weakness, numbness, or speech difficulties occur, as these may indicate a transient ischemic attack (TIA) requiring urgent evaluation to prevent stroke. Persistent confusion, loss of consciousness, or repetitive jerking movements without recovery between episodes suggest a seizure needing prompt diagnosis and treatment. Emergency signs for both conditions include sudden vision changes, severe headache, and difficulty breathing, necessitating rapid intervention to reduce complications.
Transient ischemic attack Infographic
 libterm.com
libterm.com