Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility. It commonly affects the knees, hips, hands, and spine, impacting daily activities and quality of life. Discover comprehensive insights on symptoms, treatment options, and management strategies to help you navigate this condition effectively.
Table of Comparison
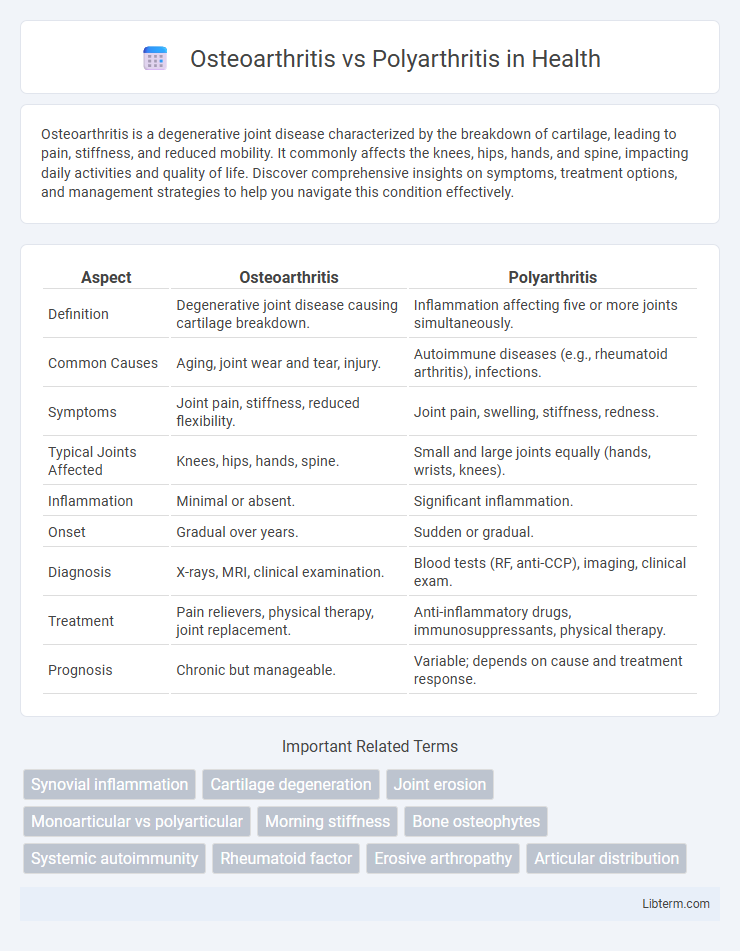
| Aspect | Osteoarthritis | Polyarthritis |
|---|---|---|
| Definition | Degenerative joint disease causing cartilage breakdown. | Inflammation affecting five or more joints simultaneously. |
| Common Causes | Aging, joint wear and tear, injury. | Autoimmune diseases (e.g., rheumatoid arthritis), infections. |
| Symptoms | Joint pain, stiffness, reduced flexibility. | Joint pain, swelling, stiffness, redness. |
| Typical Joints Affected | Knees, hips, hands, spine. | Small and large joints equally (hands, wrists, knees). |
| Inflammation | Minimal or absent. | Significant inflammation. |
| Onset | Gradual over years. | Sudden or gradual. |
| Diagnosis | X-rays, MRI, clinical examination. | Blood tests (RF, anti-CCP), imaging, clinical exam. |
| Treatment | Pain relievers, physical therapy, joint replacement. | Anti-inflammatory drugs, immunosuppressants, physical therapy. |
| Prognosis | Chronic but manageable. | Variable; depends on cause and treatment response. |
Understanding Osteoarthritis: Definition and Causes
Osteoarthritis is a degenerative joint disease characterized by the gradual breakdown of cartilage, leading to pain, stiffness, and reduced mobility. It primarily results from age-related wear and tear, joint injury, or repetitive stress on the joints, affecting commonly the knees, hips, hands, and spine. Unlike polyarthritis, which involves inflammation in multiple joints often due to autoimmune conditions, osteoarthritis is mainly a mechanical disorder with localized joint deterioration.
What is Polyarthritis? Key Characteristics
Polyarthritis is a medical condition characterized by inflammation in five or more joints simultaneously, often affecting symmetrical joints such as those in the hands, wrists, and knees. This condition can result from autoimmune diseases like rheumatoid arthritis or infections, leading to pain, stiffness, swelling, and reduced joint mobility. Unlike osteoarthritis, which typically involves wear-and-tear damage primarily in weight-bearing joints, polyarthritis involves widespread inflammatory processes affecting multiple joint sites.
Differences Between Osteoarthritis and Polyarthritis
Osteoarthritis primarily involves the degeneration of cartilage in individual joints, leading to localized pain and stiffness, whereas polyarthritis affects multiple joints simultaneously, often due to autoimmune or inflammatory conditions. Osteoarthritis is characterized by wear-and-tear changes visible in joint X-rays, while polyarthritis commonly presents with systemic symptoms and elevated inflammatory markers like ESR and CRP. Treatment approaches differ, with osteoarthritis focusing on pain management and joint preservation, and polyarthritis often requiring immunosuppressive or disease-modifying antirheumatic drugs (DMARDs).
Common Symptoms: Osteoarthritis vs Polyarthritis
Osteoarthritis commonly presents with joint pain, stiffness, and reduced mobility primarily in weight-bearing joints such as the knees, hips, and hands. Polyarthritis typically involves inflammation in multiple joints simultaneously, often symmetric, causing swelling, tenderness, and prolonged morning stiffness. Both conditions share symptoms like joint discomfort and decreased function but differ markedly in underlying pathology and systemic manifestations.
Risk Factors and Predisposing Conditions
Osteoarthritis primarily develops due to aging, joint injury, obesity, and repetitive stress on the joints, with risk factors including older age, female gender, and a history of joint trauma. Polyarthritis often results from autoimmune conditions such as rheumatoid arthritis or lupus, with genetic predisposition, female sex, and environmental triggers like smoking significantly increasing susceptibility. Both conditions are influenced by systemic inflammation, but osteoarthritis is characterized by cartilage degeneration while polyarthritis involves multiple joint inflammation caused by immune dysregulation.
Diagnosing Osteoarthritis and Polyarthritis
Diagnosing osteoarthritis primarily involves clinical evaluation of joint pain, stiffness, and crepitus, supported by imaging techniques such as X-rays that reveal joint space narrowing, osteophyte formation, and subchondral sclerosis. Polyarthritis diagnosis requires comprehensive assessment including laboratory tests like rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) to detect systemic inflammation, alongside imaging modalities like ultrasound or MRI to evaluate synovial inflammation and joint erosion in multiple joints. Differentiating osteoarthritis from polyarthritis hinges on these diagnostic criteria, with osteoarthritis typically showing localized degenerative changes and polyarthritis presenting with systemic inflammatory markers and symmetrical joint involvement.
Treatment Options for Osteoarthritis
Osteoarthritis treatment primarily involves pain management through NSAIDs, physical therapy, and lifestyle modifications such as weight loss and exercise to improve joint function. In advanced cases, intra-articular corticosteroid injections or hyaluronic acid may be used to reduce inflammation and enhance lubrication. Surgical options like joint replacement become viable when conservative treatments fail to alleviate severe joint degeneration.
Managing Polyarthritis: Therapies and Approaches
Managing polyarthritis involves a combination of disease-modifying antirheumatic drugs (DMARDs), biologic agents, and physical therapy to reduce inflammation, control symptoms, and prevent joint damage. Rheumatologists tailor treatments based on the specific type of polyarthritis, such as rheumatoid arthritis or psoriatic arthritis, often incorporating corticosteroids for short-term flare control. Regular monitoring and lifestyle modifications, including exercise and diet, play crucial roles in improving patient outcomes and maintaining joint function.
Lifestyle Modifications for Joint Health
Lifestyle modifications for osteoarthritis emphasize low-impact exercises like swimming and cycling to maintain joint mobility while reducing strain. In polyarthritis, balanced physical activity combined with tailored strength training preserves joint function and minimizes inflammation. Both conditions benefit from weight management, a balanced diet rich in omega-3 fatty acids, and ergonomic adjustments to daily activities to support overall joint health.
Prognosis and Long-term Outlook
Osteoarthritis prognosis generally involves gradual joint degeneration with manageable symptoms through lifestyle modifications and medication, while polyarthritis, often linked to autoimmune conditions like rheumatoid arthritis, poses a more variable long-term outlook depending on disease severity and treatment efficacy. Early diagnosis and consistent treatment in polyarthritis can slow disease progression and improve quality of life, whereas osteoarthritis progression is typically slower and less influenced by systemic therapies. Chronic inflammation in polyarthritis increases the risk of joint damage and disability, whereas osteoarthritis primarily results in localized wear and tear with less systemic impact.
Osteoarthritis Infographic
 libterm.com
libterm.com