Adenoidectomy is a surgical procedure that removes the adenoids, which are lymphatic tissue located behind the nasal cavity. This operation can alleviate breathing difficulties, chronic infections, and sleep apnea commonly caused by enlarged or infected adenoids. Discover more about the benefits, risks, and recovery process by reading the full article.
Table of Comparison
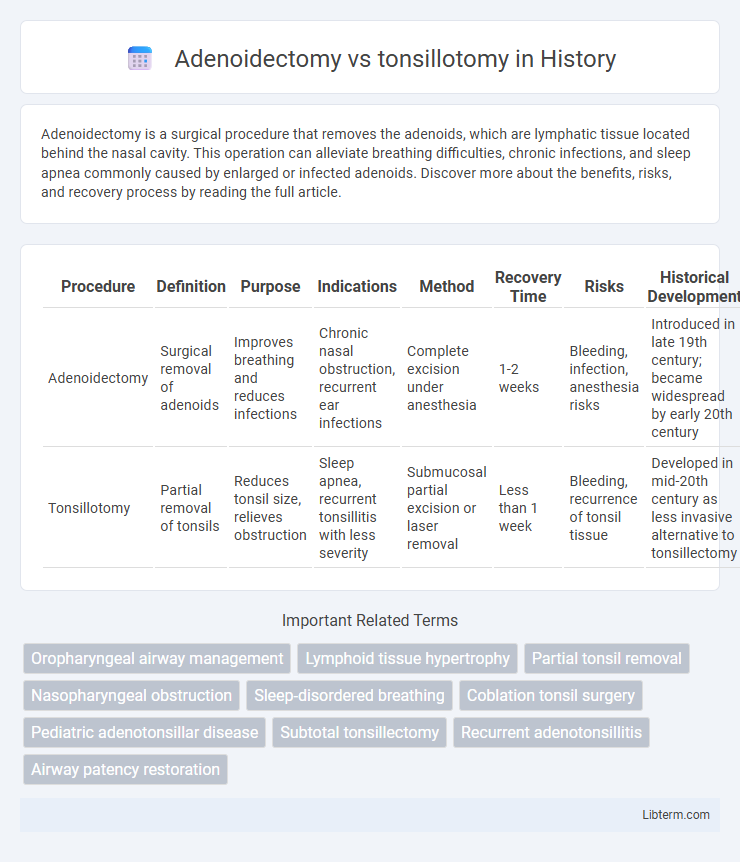
| Procedure | Definition | Purpose | Indications | Method | Recovery Time | Risks | Historical Development |
|---|---|---|---|---|---|---|---|
| Adenoidectomy | Surgical removal of adenoids | Improves breathing and reduces infections | Chronic nasal obstruction, recurrent ear infections | Complete excision under anesthesia | 1-2 weeks | Bleeding, infection, anesthesia risks | Introduced in late 19th century; became widespread by early 20th century |
| Tonsillotomy | Partial removal of tonsils | Reduces tonsil size, relieves obstruction | Sleep apnea, recurrent tonsillitis with less severity | Submucosal partial excision or laser removal | Less than 1 week | Bleeding, recurrence of tonsil tissue | Developed in mid-20th century as less invasive alternative to tonsillectomy |
Introduction to Adenoidectomy and Tonsillotomy
Adenoidectomy involves the surgical removal of the adenoid glands located behind the nasal cavity, primarily to treat recurrent infections or breathing difficulties. Tonsillotomy is a partial removal of the tonsils, typically performed to reduce obstruction while preserving some lymphatic tissue. Both procedures address upper airway issues but differ in the extent of tissue removal and recovery profiles.
Anatomical Differences: Adenoids vs Tonsils
Adenoidectomy targets the adenoids, lymphatic tissue located in the nasopharynx behind the nasal cavity, whereas tonsillotomy involves partial removal of the palatine tonsils situated on either side of the oropharynx. The adenoids play a crucial role in filtering airborne pathogens during early childhood, while the tonsils act as the first line of immune defense against ingested or inhaled microbes. Anatomically, adenoids are embedded in the nasopharyngeal mucosa and often inaccessible through the mouth, necessitating different surgical approaches compared to the more externally visible and accessible tonsils.
Indications for Adenoidectomy
Adenoidectomy is primarily indicated for children experiencing recurrent or chronic adenoid infections, persistent nasal obstruction causing breathing difficulties, or sleep-disordered breathing such as obstructive sleep apnea. It is also recommended when adenoids contribute to chronic otitis media with effusion leading to hearing impairment. Unlike tonsillotomy, which is often reserved for tonsillar hypertrophy with obstructive symptoms, adenoidectomy targets the removal of hypertrophic or infected adenoidal tissue impacting nasal airway and Eustachian tube function.
Indications for Tonsillotomy
Tonsillotomy is primarily indicated for children suffering from obstructive sleep apnea (OSA) due to hypertrophic tonsils, providing symptom relief while preserving tonsillar tissue. This procedure is preferred in cases where recurrent infections are minimal or absent, reducing post-operative pain and bleeding risks compared to full tonsillectomy. Tonsillotomy offers an effective alternative for managing airway obstruction with lower complication rates, especially in pediatric patients under 7 years old.
Surgical Techniques Compared
Adenoidectomy involves the complete removal of the adenoids using curettage or electrocautery, while tonsillotomy uses partial removal of the tonsils with techniques such as microdebrider, laser, or coblation for tissue reduction. Adenoidectomy is typically performed under general anesthesia with an emphasis on minimizing intraoperative bleeding, whereas tonsillotomy aims to preserve tonsillar tissue to reduce postoperative pain and improve recovery time. Surgical precision and choice of technology in tonsillotomy allow for selective excision, contrasting with adenoidectomy's broader tissue removal approach targeting lymphoid hypertrophy.
Recovery Times and Postoperative Care
Adenoidectomy generally involves a longer recovery time of about 7 to 10 days compared to tonsillotomy, which typically has a faster recovery period of 3 to 5 days. Postoperative care for both procedures emphasizes pain management, hydration, and avoiding strenuous activity, but patients undergoing adenoidectomy may require more attention to nasal congestion and potential ear infections. Tonsillotomy patients often experience less severe throat pain, allowing for a quicker return to normal diet and daily activities.
Risks and Complications
Adenoidectomy carries risks such as bleeding, infection, and potential injury to surrounding tissues, while tonsillotomy presents a lower risk profile with less postoperative pain and faster recovery compared to full tonsil removal. Both procedures may cause temporary swallowing difficulties, but tonsillotomy is associated with reduced risk of severe bleeding and fewer long-term complications. Understanding these differences is crucial for choosing the optimal treatment for conditions like obstructive sleep apnea or recurrent infections.
Benefits and Long-Term Outcomes
Adenoidectomy effectively reduces recurrent ear infections and nasal obstruction by removing enlarged adenoids, with long-term benefits including improved breathing and fewer respiratory infections. Tonsillotomy preserves partial tonsil tissue, resulting in less postoperative pain and quicker recovery while maintaining immune function, making it suitable for children with obstructive sleep apnea. Studies indicate both procedures improve airway obstruction, but tonsillotomy demonstrates fewer complications and better long-term quality of life in select patients compared to traditional tonsillectomy.
Patient Selection Criteria
Patient selection criteria for adenoidectomy versus tonsillotomy primarily depend on the severity and frequency of symptoms such as recurrent infections, nasal obstruction, and sleep-disordered breathing. Adenoidectomy is typically preferred for patients with chronic adenoid hypertrophy causing nasal blockage or otitis media, while tonsillotomy is indicated for children with moderate tonsillar hypertrophy contributing to obstructive sleep apnea but without frequent tonsillitis. Assessing factors like age, comorbidities, and frequency of infections guides clinicians to choose the most effective and least invasive surgical option.
Choosing the Right Procedure
Choosing the right procedure between adenoidectomy and tonsillotomy depends on the specific diagnosis and symptoms presented. Adenoidectomy is typically recommended for chronic adenoid hypertrophy causing nasal obstruction or recurrent ear infections, while tonsillotomy is preferred for partial removal of enlarged tonsils to alleviate obstructive sleep apnea with reduced postoperative pain. Accurate assessment by an ENT specialist ensures targeted treatment for optimal airway improvement and recovery outcomes.
Adenoidectomy Infographic
 libterm.com
libterm.com