A tonsillectomy is a surgical procedure to remove the tonsils, often performed to treat recurrent tonsillitis or obstructive sleep apnea. Recovery typically involves managing throat pain and avoiding strenuous activity for about two weeks. Explore the rest of the article to learn about the benefits, risks, and recovery tips for your tonsillectomy.
Table of Comparison
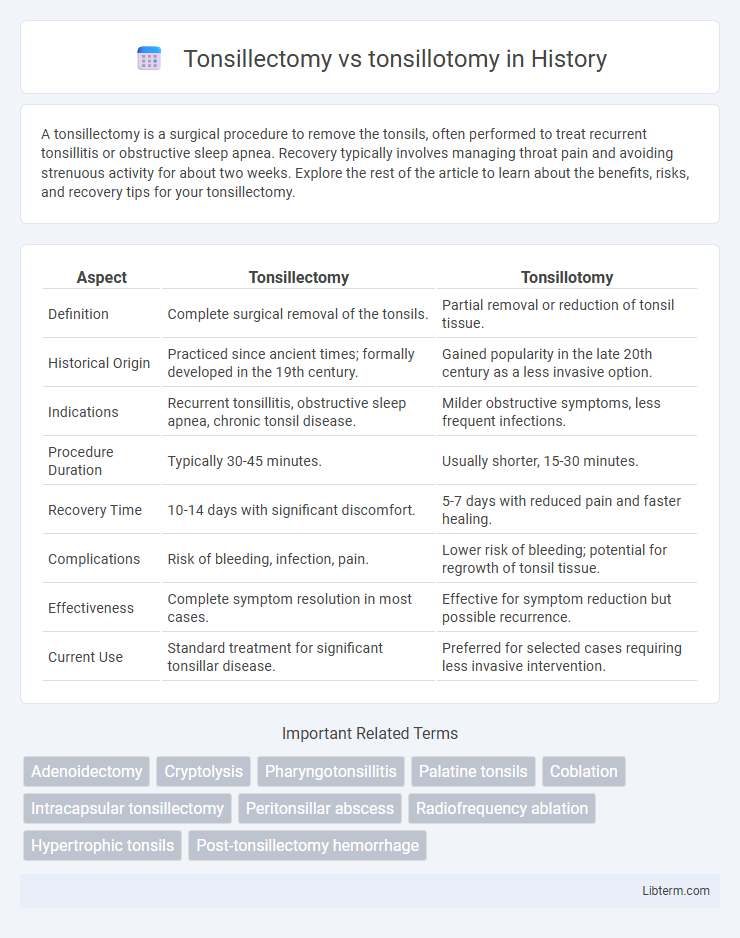
| Aspect | Tonsillectomy | Tonsillotomy |
|---|---|---|
| Definition | Complete surgical removal of the tonsils. | Partial removal or reduction of tonsil tissue. |
| Historical Origin | Practiced since ancient times; formally developed in the 19th century. | Gained popularity in the late 20th century as a less invasive option. |
| Indications | Recurrent tonsillitis, obstructive sleep apnea, chronic tonsil disease. | Milder obstructive symptoms, less frequent infections. |
| Procedure Duration | Typically 30-45 minutes. | Usually shorter, 15-30 minutes. |
| Recovery Time | 10-14 days with significant discomfort. | 5-7 days with reduced pain and faster healing. |
| Complications | Risk of bleeding, infection, pain. | Lower risk of bleeding; potential for regrowth of tonsil tissue. |
| Effectiveness | Complete symptom resolution in most cases. | Effective for symptom reduction but possible recurrence. |
| Current Use | Standard treatment for significant tonsillar disease. | Preferred for selected cases requiring less invasive intervention. |
Overview of Tonsillectomy and Tonsillotomy
Tonsillectomy involves the complete surgical removal of the tonsils, typically recommended for recurrent tonsillitis or obstructive sleep apnea. Tonsillotomy, also known as partial tonsillectomy, removes only a portion of the tonsillar tissue, preserving some tonsil function while reducing symptoms. Both procedures aim to alleviate airway obstruction and recurrent infections but differ in recovery time, complication risks, and long-term tonsil regrowth rates.
Indications for Each Procedure
Tonsillectomy is primarily indicated for recurrent tonsillitis, obstructive sleep apnea, and peritonsillar abscesses resistant to medical treatment. Tonsillotomy is preferred in cases of mild to moderate tonsillar hypertrophy causing partial airway obstruction or snoring without recurrent infections. Selecting the appropriate procedure depends on the severity of symptoms, frequency of infections, and the risk-benefit assessment of tonsil tissue removal versus reduction.
Surgical Techniques Compared
Tonsillectomy involves the complete removal of the tonsils using techniques such as cold knife dissection, electrocautery, or coblation, offering thorough disease resolution but with higher postoperative pain and bleeding risk. Tonsillotomy, or partial tonsil removal, typically utilizes microdebriders or laser tools to excise only the hypertrophic portions, resulting in less pain, faster recovery, and reduced bleeding but potential for tonsil tissue regrowth. Surgical choice depends on patient age, severity of symptoms, and risk factors, with tonsillectomy favored for recurrent infections and tonsillotomy preferred for obstructive sleep apnea with tonsillar hypertrophy.
Recovery Time and Process
Tonsillectomy typically involves complete removal of the tonsils and generally requires a recovery period of 10 to 14 days with moderate pain and a risk of bleeding. Tonsillotomy, a partial removal of tonsil tissue, usually results in a shorter recovery time of 5 to 7 days with less postoperative pain and reduced risk of complications. Both procedures demand careful wound care and hydration to promote healing and prevent infection.
Risks and Complications
Tonsillectomy involves complete removal of the tonsils and carries higher risks of bleeding, pain, and infection compared to tonsillotomy, which only removes part of the tonsillar tissue. Tonsillotomy generally results in fewer complications, reduced postoperative pain, and quicker recovery but may have a higher risk of tonsil regrowth or the return of symptoms. Both procedures risk anesthesia complications and require careful evaluation of patient history to determine the most appropriate surgical approach.
Effectiveness in Treating Recurrent Infections
Tonsillectomy completely removes the tonsils, offering a higher success rate in preventing recurrent tonsillar infections compared to tonsillotomy, which only partially removes tonsillar tissue. Studies indicate tonsillectomy results in significantly fewer postoperative infections and reduced need for additional surgeries. Tonsillotomy may be preferred for less severe cases or to reduce recovery time, but it generally shows lower long-term effectiveness in eliminating recurrent infections.
Impact on Sleep Apnea and Breathing
Tonsillectomy, the complete removal of tonsils, significantly improves airway obstruction and reduces symptoms of obstructive sleep apnea (OSA) in both children and adults by eliminating enlarged tonsillar tissue. Tonsillotomy, a partial removal procedure, also alleviates breathing difficulties and mild to moderate OSA but retains some tonsillar tissue, which may reduce postoperative pain and recovery time. Studies show tonsillectomy provides greater long-term resolution of severe sleep apnea, while tonsillotomy is favorable for patients requiring less aggressive treatment with fewer complications.
Postoperative Pain and Discomfort
Postoperative pain and discomfort differ significantly between tonsillectomy and tonsillotomy, with tonsillotomy generally resulting in less pain due to partial removal of tonsillar tissue. Tonsillectomy, involving complete excision of the tonsils, typically leads to more intense throat pain lasting 7 to 10 days, requiring stronger analgesics and extended recovery. Reduced postoperative pain in tonsillotomy often enables faster return to normal diet and activities, making it preferable for patients prioritizing minimal discomfort.
Long-term Outcomes and Recurrence Rates
Tonsillectomy involves complete removal of the tonsils and generally results in lower recurrence rates of tonsillar disease compared to tonsillotomy, which only partially removes tissue. Long-term outcomes indicate that tonsillectomy patients experience fewer episodes of tonsillitis and less need for reoperation, while tonsillotomy may preserve some immune function but carries a higher likelihood of symptom recurrence. Clinical studies show recurrence rates after tonsillotomy range from 10% to 20%, whereas tonsillectomy recurrence is typically below 5%, highlighting a trade-off between tissue preservation and long-term efficacy.
Choosing the Right Surgery: Factors to Consider
Choosing between tonsillectomy and tonsillotomy depends on factors such as the severity of symptoms, patient age, and risk of complications. Tonsillectomy, involving complete removal of tonsils, is preferred for recurrent infections and large obstructive tonsils, while tonsillotomy, partial removal, is often considered for less severe cases with emphasis on quicker recovery. Evaluating medical history, frequency of infections, and potential surgical risks is crucial in determining the appropriate procedure.
Tonsillectomy Infographic
 libterm.com
libterm.com