Pathogenic organisms have the ability to cause disease by invading the host and disrupting normal biological functions. Understanding the mechanisms of pathogenicity helps in developing effective treatments and preventive measures. Explore the rest of this article to learn how pathogens impact health and how you can protect yourself.
Table of Comparison
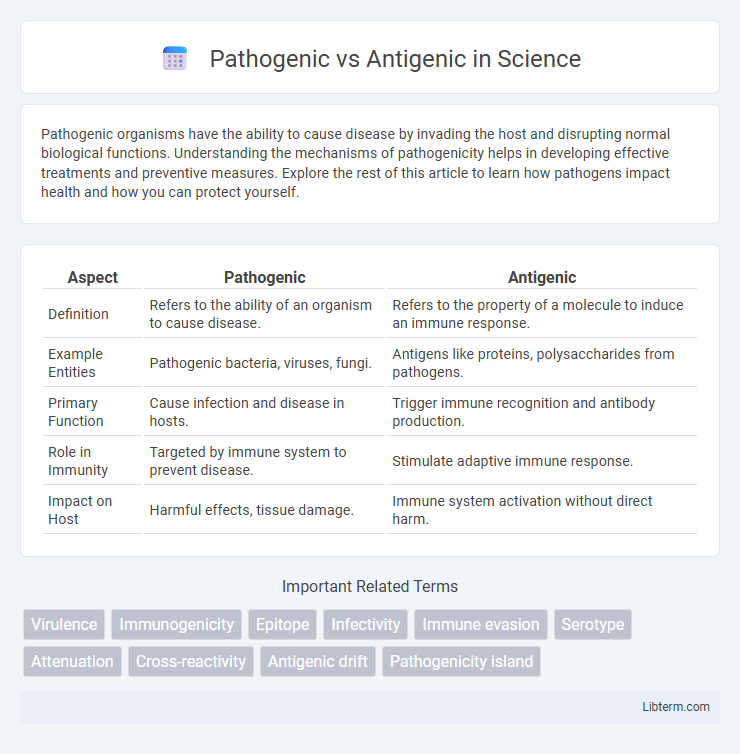
| Aspect | Pathogenic | Antigenic |
|---|---|---|
| Definition | Refers to the ability of an organism to cause disease. | Refers to the property of a molecule to induce an immune response. |
| Example Entities | Pathogenic bacteria, viruses, fungi. | Antigens like proteins, polysaccharides from pathogens. |
| Primary Function | Cause infection and disease in hosts. | Trigger immune recognition and antibody production. |
| Role in Immunity | Targeted by immune system to prevent disease. | Stimulate adaptive immune response. |
| Impact on Host | Harmful effects, tissue damage. | Immune system activation without direct harm. |
Understanding Pathogenicity and Antigenicity
Pathogenicity refers to the ability of a microorganism to cause disease, determined by factors such as virulence, invasion, and toxin production. Antigenicity is the capacity of a pathogen to be recognized by the host's immune system, specifically through the identification of antigens that trigger an immune response. Understanding the distinction between pathogenicity and antigenicity is crucial for developing effective vaccines and therapeutic strategies targeting infection mechanisms and immune recognition.
Key Differences Between Pathogenic and Antigenic Agents
Pathogenic agents are microorganisms such as bacteria, viruses, fungi, or parasites that cause diseases in their hosts by invading tissues and disrupting normal functions. Antigenic agents refer to substances, often proteins or polysaccharides on the surface of pathogens, that trigger an immune response by being recognized as foreign by the host's immune system. The key difference lies in their roles: pathogenic agents directly cause infection and illness, while antigenic agents elicit immune detection and response without necessarily causing disease themselves.
The Role of Pathogens in Infectious Diseases
Pathogens, including bacteria, viruses, fungi, and parasites, play a central role in infectious diseases by invading host organisms and disrupting normal biological functions. Their ability to cause disease depends on factors such as virulence, immune evasion, and toxin production, distinguishing them from antigens, which are molecules that trigger immune responses without necessarily causing disease. Understanding pathogen mechanisms facilitates the development of targeted treatments and vaccines to control infectious diseases effectively.
How Antigens Trigger Immune Responses
Antigens are molecules typically found on the surface of pathogens that the immune system recognizes as foreign, triggering a specific immune response. These molecules bind to receptors on immune cells such as B cells and T cells, leading to the activation and proliferation of these cells to target and eliminate the pathogen. Unlike pathogenic factors that cause disease directly, antigens primarily serve as signals to activate adaptive immunity, including the production of antibodies and memory cells for long-term protection.
Mechanisms of Pathogenicity in Microorganisms
Pathogenic microorganisms employ mechanisms such as toxin production, adhesion to host cells, invasion, and immune system evasion to cause disease by damaging host tissues. Antigenic properties refer to the ability of microbial molecules, like surface proteins, to be recognized by the host immune system, triggering an immune response without necessarily causing disease. Understanding the distinction between pathogenicity mechanisms and antigenicity is crucial for developing vaccines that target microbial antigens while mitigating pathogenic effects.
Antigenic Variation and Immune Evasion
Antigenic variation is a critical mechanism by which pathogens alter surface proteins to evade host immune responses, enabling persistent infections and complicating vaccine development. This process involves genetic changes such as gene conversion, mutation, or recombination, resulting in altered antigenic profiles that escape recognition by antibodies and T cells. Understanding antigenic variation enhances insights into immune evasion strategies and informs the design of effective immunotherapies against rapidly evolving pathogens.
Clinical Implications: Pathogenicity vs Antigenicity
Pathogenicity refers to the ability of a microorganism to cause disease, influencing clinical management through infection severity, treatment strategies, and prognosis. Antigenicity involves the capacity of a pathogen's components to trigger an immune response, impacting vaccine design, diagnostic accuracy, and immunotherapy development. Understanding the distinction between pathogenicity and antigenicity is critical for developing effective clinical interventions and public health measures.
Diagnostic Approaches for Pathogens and Antigens
Diagnostic approaches for pathogens primarily involve direct detection techniques such as polymerase chain reaction (PCR), culture methods, and microscopy to identify and characterize infectious agents at the molecular or cellular level. Antigenic detection methods focus on identifying specific proteins or molecular markers of pathogens using immunoassays like enzyme-linked immunosorbent assay (ELISA) and rapid antigen tests, which provide rapid and specific results. Combining both pathogen detection and antigenic profiling enhances diagnostic accuracy, guiding targeted treatment and epidemiological surveillance.
Vaccine Development: Targeting Pathogenic and Antigenic Factors
Vaccine development targets pathogenic factors such as virulence proteins and toxins that directly contribute to disease severity, aiming to neutralize or eliminate these harmful agents to prevent infection. Antigenic factors, including surface proteins and polysaccharides, serve as molecular signatures recognized by the immune system, guiding the design of vaccines that elicit strong, specific immune responses. Understanding the distinction between pathogenicity and antigenicity enables the creation of vaccines that effectively block pathogen entry and stimulate long-lasting immunity.
Future Research in Pathogenicity and Antigenicity
Future research in pathogenicity and antigenicity will likely emphasize advanced genomic and proteomic analyses to identify novel virulence factors and immune evasion mechanisms. Emerging techniques such as CRISPR-Cas9 gene editing and single-cell RNA sequencing are expected to elucidate pathogen-host interactions at unprecedented resolution. These insights could drive the development of next-generation vaccines and targeted therapeutics with enhanced efficacy against evolving infectious agents.
Pathogenic Infographic
 libterm.com
libterm.com