Cellulitis is a common bacterial skin infection causing redness, swelling, and pain, often requiring prompt medical treatment to prevent complications. It typically affects the lower legs but can occur anywhere on the body, especially where the skin has been broken. Discover essential insights to protect your health and understand the best steps for treatment by reading the full article.
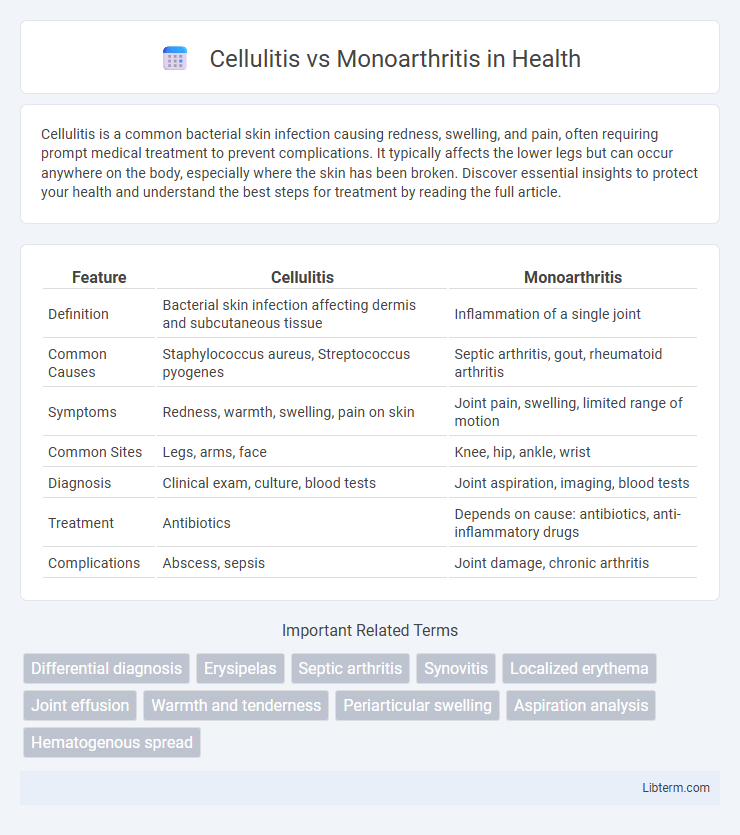
Table of Comparison
| Feature | Cellulitis | Monoarthritis |
|---|---|---|
| Definition | Bacterial skin infection affecting dermis and subcutaneous tissue | Inflammation of a single joint |
| Common Causes | Staphylococcus aureus, Streptococcus pyogenes | Septic arthritis, gout, rheumatoid arthritis |
| Symptoms | Redness, warmth, swelling, pain on skin | Joint pain, swelling, limited range of motion |
| Common Sites | Legs, arms, face | Knee, hip, ankle, wrist |
| Diagnosis | Clinical exam, culture, blood tests | Joint aspiration, imaging, blood tests |
| Treatment | Antibiotics | Depends on cause: antibiotics, anti-inflammatory drugs |
| Complications | Abscess, sepsis | Joint damage, chronic arthritis |
Overview of Cellulitis and Monoarthritis
Cellulitis is a common bacterial skin infection characterized by redness, swelling, warmth, and pain, primarily affecting the deeper layers of the skin and subcutaneous tissues. Monoarthritis refers to inflammation of a single joint, presenting with pain, swelling, and limited range of motion often caused by infection, trauma, or autoimmune conditions. Differentiating cellulitis from monoarthritis involves clinical evaluation and diagnostic imaging to identify skin infection versus joint involvement.
Causes and Risk Factors
Cellulitis is caused by bacterial infection, commonly Streptococcus or Staphylococcus species, entering through skin breaks, with risk factors including diabetes, immunosuppression, and chronic edema. Monoarthritis results from joint inflammation due to infections (septic arthritis), crystal deposition (gout or pseudogout), or trauma, with risk factors involving joint injury, pre-existing joint disease, and immunocompromised states. Both conditions share risk factors like compromised immunity but differ fundamentally in infection site and inflammatory mechanism.
Key Clinical Differences
Cellulitis presents as a diffuse, tender, erythematous skin infection often accompanied by fever and systemic symptoms, while monoarthritis involves localized joint inflammation characterized by pain, swelling, limited range of motion, and possible effusion. Cellulitis typically affects the dermis and subcutaneous tissues, whereas monoarthritis primarily affects a single joint, commonly the knee or ankle, with signs of joint effusion and warmth. Diagnostic differentiation relies on clinical examination, imaging, and laboratory tests such as elevated inflammatory markers for both, but joint aspiration with synovial fluid analysis is crucial for confirming monoarthritis and ruling out septic arthritis.
Common Signs and Symptoms
Cellulitis presents with localized skin redness, warmth, swelling, and pain, often accompanied by fever and chills. Monoarthritis typically causes joint pain, swelling, stiffness, and limited range of motion, usually affecting a single joint. Both conditions may exhibit inflammation, but cellulitis predominantly affects the skin and subcutaneous tissues, whereas monoarthritis involves the synovial joint.
Diagnostic Approaches
Diagnostic approaches for cellulitis primarily involve clinical evaluation of erythema, warmth, swelling, and pain, supported by laboratory tests such as elevated white blood cell count and C-reactive protein levels. In contrast, monoarthritis diagnosis relies on joint aspiration and synovial fluid analysis to detect infection, crystals, or inflammatory markers, alongside imaging studies like X-rays or ultrasound to identify joint effusion or bone involvement. Blood cultures and skin biopsy may aid in differentiating cellulitis from septic arthritis in ambiguous cases.
Laboratory and Imaging Findings
Laboratory findings in cellulitis typically show elevated white blood cell count and increased C-reactive protein, indicative of systemic infection, whereas monoarthritis often reveals synovial fluid analysis with elevated leukocytes and possible crystals in gout. Imaging for cellulitis primarily includes ultrasound to assess soft tissue swelling and exclude abscess formation, while monoarthritis relies on X-rays to detect joint space narrowing, erosions, or effusions, with MRI providing detailed evaluation of joint inflammation and cartilage damage. Blood cultures may be positive in cellulitis but are usually negative in monoarthritis unless septic arthritis is present.
Treatment Strategies
Cellulitis treatment primarily involves systemic antibiotics targeting common causative bacteria such as Streptococcus pyogenes and Staphylococcus aureus, with first-line options including cephalexin or clindamycin for penicillin-allergic patients. Monoarthritis requires addressing the underlying cause; septic arthritis necessitates prompt joint aspiration, intravenous antibiotics like vancomycin or ceftriaxone, and sometimes surgical drainage, while non-infectious forms are managed with anti-inflammatory medications or disease-specific therapies. Early differentiation through clinical evaluation, laboratory tests, and imaging guides targeted treatment strategies to optimize outcomes and prevent complications.
Complications and Prognosis
Cellulitis can lead to serious complications such as abscess formation, sepsis, and chronic swelling if untreated, with prognosis generally favorable when promptly managed with antibiotics. Monoarthritis, often caused by infection or crystal deposition, risks joint destruction and chronic disability if diagnosis and treatment are delayed, making early intervention critical for preserving joint function. Both conditions require accurate differentiation to prevent long-term sequelae and ensure optimal recovery outcomes.
Prevention and Patient Education
Prevention of cellulitis involves proper skin care, including regular cleansing, moisturizing, and prompt treatment of wounds or insect bites to reduce bacterial entry points. Educating patients on recognizing early signs of cellulitis, such as redness, swelling, and warmth, enhances timely medical intervention and reduces complications. For monoarthritis, patient education emphasizes joint protection, avoiding repetitive trauma, and seeking early evaluation of joint pain and swelling to prevent joint damage and chronic inflammation.
When to Seek Immediate Medical Attention
Seek immediate medical attention for cellulitis if you experience rapidly spreading redness, severe pain, swelling, fever above 101degF (38.3degC), or signs of systemic infection such as confusion or difficulty breathing. In monoarthritis, urgent care is necessary when there is sudden, intense joint pain accompanied by swelling, redness, fever, or inability to move the joint, as these may indicate septic arthritis requiring prompt treatment. Early medical intervention is crucial to prevent complications like abscess formation in cellulitis or joint destruction in septic monoarthritis.
Cellulitis Infographic
 libterm.com
libterm.com