A laryngectomy is a surgical procedure that involves the removal of the larynx, typically performed to treat laryngeal cancer or severe trauma. This surgery results in significant changes to breathing, speech, and swallowing, requiring adaptation through rehabilitation and speech therapy. Explore the article to understand the procedure, recovery process, and how to manage life after a laryngectomy.
Table of Comparison
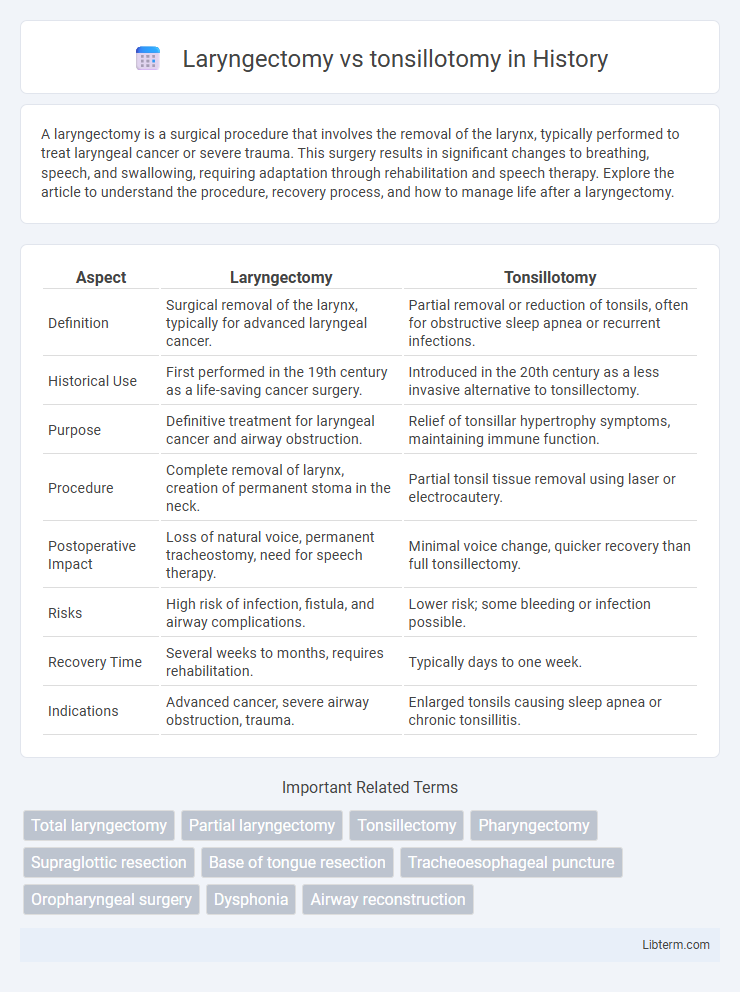
| Aspect | Laryngectomy | Tonsillotomy |
|---|---|---|
| Definition | Surgical removal of the larynx, typically for advanced laryngeal cancer. | Partial removal or reduction of tonsils, often for obstructive sleep apnea or recurrent infections. |
| Historical Use | First performed in the 19th century as a life-saving cancer surgery. | Introduced in the 20th century as a less invasive alternative to tonsillectomy. |
| Purpose | Definitive treatment for laryngeal cancer and airway obstruction. | Relief of tonsillar hypertrophy symptoms, maintaining immune function. |
| Procedure | Complete removal of larynx, creation of permanent stoma in the neck. | Partial tonsil tissue removal using laser or electrocautery. |
| Postoperative Impact | Loss of natural voice, permanent tracheostomy, need for speech therapy. | Minimal voice change, quicker recovery than full tonsillectomy. |
| Risks | High risk of infection, fistula, and airway complications. | Lower risk; some bleeding or infection possible. |
| Recovery Time | Several weeks to months, requires rehabilitation. | Typically days to one week. |
| Indications | Advanced cancer, severe airway obstruction, trauma. | Enlarged tonsils causing sleep apnea or chronic tonsillitis. |
Introduction to Laryngectomy and Tonsillotomy
Laryngectomy is a surgical procedure involving the partial or total removal of the larynx, commonly performed to treat advanced laryngeal cancer, enabling airway management and voice restoration. Tonsillotomy, on the other hand, is a partial removal of the tonsils typically indicated for recurrent tonsillitis or obstructive sleep apnea, preserving some tonsillar tissue to maintain immune function. Both surgeries address distinct anatomical structures within the upper airway and have different clinical indications and outcomes.
Understanding the Procedures: Laryngectomy vs Tonsillotomy
Laryngectomy involves the surgical removal of the larynx, typically performed to treat advanced laryngeal cancer, resulting in permanent voice loss and a tracheostomy for breathing. Tonsillotomy, on the other hand, is a partial removal of the tonsils primarily used to treat chronic tonsillitis or sleep apnea while preserving some tonsillar tissue to maintain immune function. Understanding these procedures highlights the significant differences in invasiveness, recovery, and long-term impacts on speech and respiratory function.
Indications for Laryngectomy
Laryngectomy is primarily indicated for advanced laryngeal cancer, particularly when tumors involve deep tissue or cartilage invasion, making conservative treatments ineffective. It is also performed in cases of irreversible laryngeal trauma, severe airway obstruction, or recurrent tumors after radiation therapy failure. In contrast, tonsillotomy is a less invasive procedure mainly used for partial removal of hypertrophic tonsils, primarily to improve airway obstruction or recurrent infections but not for malignant conditions.
Indications for Tonsillotomy
Tonsillotomy is primarily indicated for patients with obstructive sleep apnea, recurrent tonsillitis, or tonsillar hypertrophy causing airway obstruction without complete tonsil removal. Unlike laryngectomy, which is reserved for advanced laryngeal cancer or severe airway compromise, tonsillotomy provides symptom relief while preserving tonsillar tissue to maintain immune function. This procedure is favored in pediatric cases to reduce postoperative morbidity and preserve the tonsillar crypt anatomy.
Surgical Techniques Compared
Laryngectomy involves the complete or partial removal of the larynx, typically performed to treat advanced laryngeal cancer, using techniques such as total or partial laryngectomy with careful preservation of surrounding structures to maintain airway function. Tonsillotomy, or partial tonsillectomy, is a less invasive procedure that removes only a portion of the tonsillar tissue, often performed using microdebriders or laser technology to minimize bleeding and postoperative pain. Both surgeries require precise anatomical knowledge and differ significantly in operative complexity, risk profile, and recovery protocols due to their target tissues and underlying indications.
Risks and Complications of Each Procedure
Laryngectomy carries significant risks such as permanent loss of natural voice, potential airway complications, and infections at the surgical site. Tonsillotomy, being less invasive, primarily risks bleeding, infection, and postoperative pain, with a lower chance of airway obstruction compared to tonsillectomy. Both procedures require careful postoperative monitoring to manage complications and ensure optimal recovery.
Recovery and Postoperative Care
Recovery after a laryngectomy typically involves a longer hospital stay and intensive postoperative care, including wound management, respiratory support via tracheostomy, and speech rehabilitation. Tonsillotomy, being less invasive, generally allows for quicker recovery with minimal postoperative pain and a shorter duration of restricted diet and activity. Postoperative care for tonsillotomy focuses on pain control, hydration, and monitoring for bleeding, whereas laryngectomy requires comprehensive airway management and ongoing multidisciplinary support.
Impact on Quality of Life
Laryngectomy significantly alters voice production, swallowing, and breathing, potentially leading to challenges in communication and social interaction that affect quality of life. Tonsillotomy, a less invasive procedure, generally results in quicker recovery with minimal impact on speech and swallowing functions, preserving daily activities and comfort. Studies indicate that while laryngectomy patients often require extensive rehabilitation and assistive devices, tonsillotomy patients experience fewer postoperative complications, contributing to overall higher immediate quality of life.
Long-term Outcomes and Prognosis
Laryngectomy, typically performed for advanced laryngeal cancer, results in permanent loss of natural voice but offers significant long-term survival benefits with appropriate cancer control. Tonsillotomy, a partial removal of tonsil tissue primarily used to treat obstructive sleep apnea or recurrent infections, preserves immune function and generally has minimal long-term complications or impact on quality of life. Prognosis after laryngectomy depends heavily on cancer stage and post-operative rehabilitation, whereas tonsillotomy prognosis is favorable with rapid recovery and low risk of recurrence or chronic issues.
Choosing the Right Procedure: Key Considerations
Choosing between laryngectomy and tonsillotomy depends on the severity and location of the pathology; laryngectomy is often indicated for advanced laryngeal cancer requiring removal of the entire larynx, while tonsillotomy is typically performed for partial removal of hypertrophic tonsils causing obstructive symptoms. Patient factors such as age, overall health, and potential impact on voice and airway function are critical in determining the best surgical approach. Surgical risks, recovery time, and long-term functional outcomes, including speech and swallowing capabilities, must be carefully evaluated to ensure optimal patient-centered care.
Laryngectomy Infographic
 libterm.com
libterm.com